Cancer has been estimated as the cause of 1 in every 6 deaths worldwide. Yet less than 10% of people with cancer benefit from currently available treatments, according to an updated analysis published last year and several earlier studies.
Based in Tel Aviv, Israel, Pangea Biomed, the developer of a platform designed to predict responses to immune-oncology therapies, says its technology can increase the percentage of patients that benefit from such treatments by more than 50%.
That improvement, Pangea says, occurs through its ENLIGHT platform, designed to predict patient response to more than 100 oncology drugs that are designed to treat dozens of types of cancer. ENLIGHT uses a two-layer, transcriptomics-based computational approach to predict the effectiveness of cancer therapies on individual patients in multiple cancer types by identifying clinically relevant genomic interactions.
Using a proprietary ENLIGHT Matching Score (EMS), oncologists can identify a treatment’s efficacy potential for each individual patient, regardless of cancer type.
ENLIGHT combines data from RNA sequencing with data network effects enabled through machine learning (ML), with the aim of creating a “social graph” of genes that reveals biological insights designed to pinpoint the best option for treating cancer in patients. The platform eschews assessment of individual genes in favor of analyzing the interactions of groups of genes tied to specific cancers.
“Typically we look at groups of around 100 genes, but that’s the plain vanilla model. If you want to dive deep into one particular drug or into one particular indication, you can often trim those down and find subgroups which are more important,” Pangea CEO Tuvik Beker, PhD, said.
“If we look at the 100 most significant genes, we usually get a very robust predictive signature. But if we need to turn that into a readily available test, we can trim that down usually to 12-20 genes that are the most important and provide 95% of the predictive power.”
In ENLIGHT’s foundational layer, which Pangea calls its “inference engine,” the platform maps functional interactions between pairs of genes on a genome-wide basis.
ENLIGHT takes large amounts of data about cancer from multiple sources—including in vitro screens, drug screens, gene knockdowns with short-hairpin RNA (shRNA) or small interfering RNA (siRNA), CRISPR knockouts, genetic manipulation screens, as well as clinical data about patients’ genetic composition, gene expression, and survival rates.
Seeking Relationships
“We find evidence in that big data for functional relationships between pairs of genes in the genome, and we do that in in a way that is not specifically tied to just one cancer indication or just one particular drug,” Beker explained. “We are essentially building the social graph of cancer-related genes. We try to understand which genes are helping others, which genes are interfering with others.”
ENLIGHT’s second layer is its predictive engine designed to identify multiple targets of a given drug, then block out the whole functional “neighborhood” surrounding these targets—potentially several dozen, or even 100 or 150 genes that are strongly interacting at the functional level with the genes that the drug is targeting and inhibiting.
“If we take a tumor sample from a patient, we can look at our map, which focuses on the neighborhood of interest. We ask, does the target of that drug have a supporting neighborhood or an opposing neighborhood? When we inhibit this target, will the genes that interact with it support our treatment, or help the tumor overcome and resist the treatment?” Beker said. “We are able to provide, very intuitively, prediction scores for how effective that would be.”
Beker was one of four corresponding authors of a preprint posted March 1 on bioRxiv detailing how ENLIGHT enabled researchers from Pangea and partner institutions to prioritize treatments for a single patient, as well as select the most likely responders in a patient cohort of clinical trials.
Assessing ENLIGHT’s performance on 21 blinded clinical trial datasets, the researchers showed that the platform had a 2.59 times higher likelihood of effectively predict treatment response across multiple therapies and cancer types than an earlier transcriptomics-based approach called SELECT. One key advantage of ENLIGHT over SELECT: The former can build relevant GI networks for all 105 FDA-approved targeted cancer drugs and immunotherapies, vs just 70 for SELECT.
ENLIGHT also performed as well as supervised predictors developed for specific indications and drugs, but on a much broader array of therapies and indications. Higher EMS scores were more closely associated with significantly better responses to treatment.
‘Limited’ Chemotherapy Utility
Among limitations acknowledged by the paper’s 29 co-authors, however: Since ENLIGHT operates on the level of drug targets, it has “very limited utility” in predicting treatment response to chemotherapies. Its prediction accuracy, they added, depends on the accuracy with which the targets of a given drug have been identified.
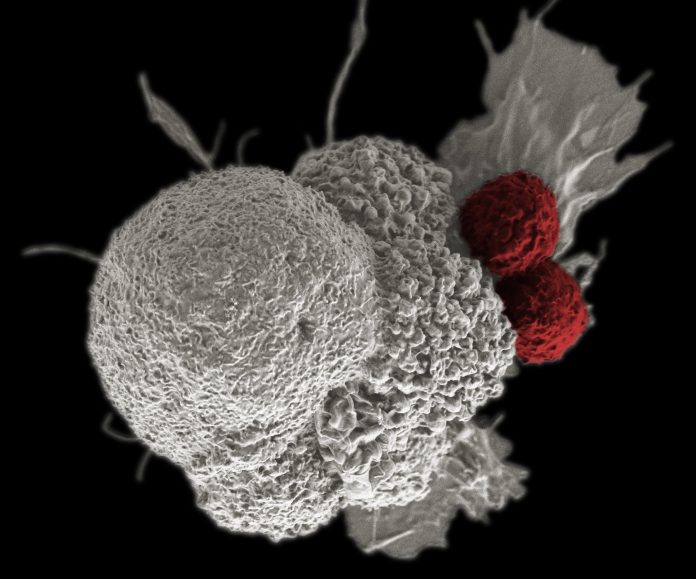
“While current applications of ENLIGHT have focused on bulk tumor transcriptomics, future work is needed to study its application to analyze single-cell tumor transcriptomics, to build predictors that consider the heterogeneity of tumors, and the important interplay between tumor and its immune microenvironment,” the researchers added.
ENLIGHT seeks out pairs of genes that show synthetic lethality—where mutation of both genes leads to cell death, but mutation of either gene alone still allows for cell viability.
“If they’re indeed a synthetic lethal pair, then what I’d expect to find when I look at thousands of human samples—and I can even do it in other organisms—is that both genes would seldom be mutually underexpressed,” Beker said. “We use all these statistical and machine learning tests to derive insights from large population-wide expression studies. There are hints in the mutual distribution functions of multiple genes. When you look at them together, and you analyze them in a proper way, you can find out the functional relationship between them.”
Pangea is among companies looking to develop tech platforms intended to facilitate precision oncology. In February, Curesponse agreed to combine its cResponse platform, also designed for accurate and timely prediction of patient response to cancer treatment, with the artificial intelligence (AI) and ML capabilities of RAFAEL Advanced Defense Systems, through a collaboration of undisclosed value.
And in November, Toronto-based Geneseeq, whose genomic profiling is designed to enable precision cancer care, announced precision oncology partnerships of undisclosed value with two pharma giants, AstraZeneca and Takeda Pharmaceutical. Geneseeq and Takeda agreed to advance lung cancer precision medicine development, standardize precision diagnostics in clinical care, improve patient access to personalized medicine, and conform to requirements of China’s “Precision Medicine Plan.”
With AstraZeneca, Geneseeq agreed with six other unnamed “industry partners” to “empower the development and application of lung cancer early screening and early diagnosis technologies,” according to a statement by Shanshan Yang, head of Geneseeq’s Early Detection Program.
Low percentages
Platform developers are looking to improve upon the low percentage of patients both eligible for, and likely to benefit from, precision oncology treatments. According to a study published 2018 in JAMA Oncology, only about 8% of cancer patients were eligible for precision oncology treatments, while just under 5% would benefit from them—up from 5% eligible and 0.7% likely to benefit in 2006. Even among patients who responded to treatment, the incremental survival benefit provided by those treatments was only measurable in months, the study found.
Last year, Haslam and two colleagues published an analysis in Annals of Oncology showing an increase in the percentage of patients who responded to genome-targeted cancer therapy—but only from 2.7% in 2006 to 7% in 2020. Most of the increase in response was seen prior to 2018, and most of the increase in eligibility after 2018.
Beker previously co-founded and remains executive chairman of MedAware, a medication safety monitoring platform, before joining Pangea in 2020 as chief technology officer, combining that role with CEO duties later that year, then becoming full-time CEO last November.
Pangea was founded in 2018 to commercialize technology that has been developed over nearly a decade. Its three co-founders are all cancer researchers: Eytan Ruppin, MD, PhD, Chief of the NCI Cancer Data Science Lab; Ze’ev Ronai, PhD, Director of the NCI-designated Cancer Center at Sanford Burnham Prebys Discovery Institute; and Eyal Gottlieb, PhD, Laura and Isaac Perlmutter Chair of Cancer Research at Technion Israel Institute of Technology.













