Scientists demonstrate an endogenously lymph node-targeting lipid nanoparticle (LNP), without the modification of any active targeting ligands, for developing an mRNA cancer vaccine. This method of targeting cancer in mice eliminated tumors and even prevented their recurrence.
This work is published in Proceedings of the National Academy of Sciences.
“What we are doing now is developing the next generation of mRNA vaccines using lipid nanoparticle delivery technology, with the ability to target specific organs and tissues,” said Qiaobing Xu, PhD, professor of biomedical engineering at Tufts School of Engineering. “Targeting the lymphatic system helped us to overcome many of the challenges that have faced others in developing a cancer vaccine.”
More than 20 mRNA cancer vaccines have been enrolled in clinical trials to date. However, much of the mRNA tends to end up in the liver. While antigens produced in the liver can still induce an immune response, there remains a risk of liver inflammation and damage. The response could be more effective and long-lasting if more of the vaccine were directed to the lymphatic system, where immune cells are concentrated.
Targeting is achieved by modifying the chemical structure of the lipids that make up the LNP. In this case, they found an LNP that concentrated in the lymph nodes after they were injected subcutaneously into mice. The researchers think the LNPs collect molecules from the blood stream on their surface, and those selected molecules bind to specific receptors in the target organ.
The cancer vaccine in this study, similar to the mRNA COVID-19 vaccines, also delivers mRNA in LNPs. The team explored an endogenously lymph node-targeting LNP named 113-O12B, which showed “increased and specific expression in the lymph node compared with LNP formulated with ALC-0315—a synthetic lipid used in the COVID-19 vaccine Comirnaty.”
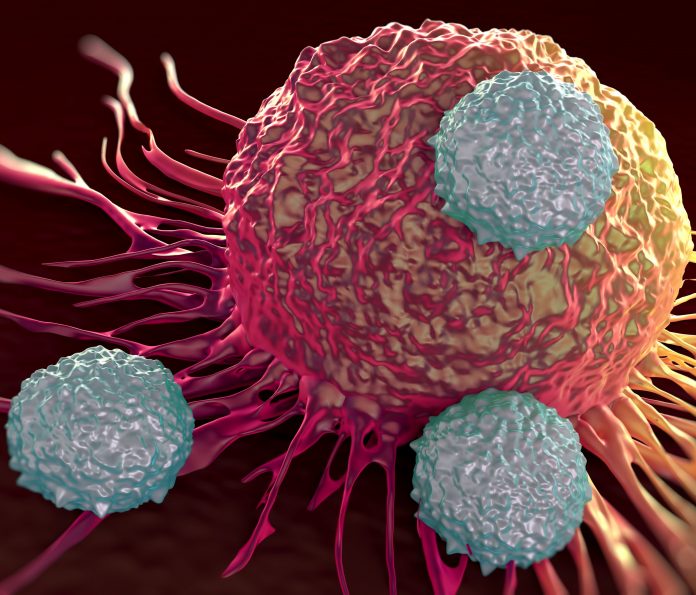
The targeted delivery of the mRNA vaccine in this study “elicits robust CD8+ T cell responses, exhibiting excellent protective and therapeutic effects on B16F10 melanoma. Notably, 113-O12B can efficiently deliver both a full-length protein and a short-peptide–based, antigens-encoded mRNA, thus providing a universal platform for mRNA vaccines.”
Mice with metastatic melanoma that were treated with the lymph-targeted vaccine showed significant inhibition of tumors and a 40% rate of complete response—no tumors—with no recurrence in the long-term when it was combined with another existing therapy that helps prevent cancer cells from suppressing an immune response.
All the mice that were in complete remission were prevented from forming any new tumors when injected later with metastatic tumor cells, showing that the cancer vaccine led to excellent immune memory.
“Cancer vaccines have always been a challenge because tumor antigens don’t always look so ‘foreign’ like antigens on viruses and bacteria, and the tumors can actively inhibit the immune response,” said Jinjin Chen, PhD, a postdoctoral research fellow in Xu’s lab. “This cancer vaccine evokes a much stronger response and is capable of carrying mRNA for both large and small antigens. We are hoping that it could become a universal platform not only for cancer vaccines, but also for more effective vaccines against viruses and other pathogens.”













