Scientists from the NIH in collaboration with UPMC Hillman Cancer Center, reporting in Science, have demonstrated in a Phase II proof-of-principal study how some patients with advanced melanoma who haven’t responded to immune checkpoint inhibitor therapy, can be converted to immunotherapy responders by giving them a fecal microbiota transplant (FMT), taken from patients who had responded very well to these treatments. The results suggest that introducing certain fecal microorganisms into a patient’s colon may help individuals respond to drugs that enhance the immune system’s ability to recognize and kill tumor cells.
“In recent years, immunotherapy drugs called PD-1 and PD-L1 inhibitors have benefited many patients with certain types of cancer, but we need new strategies to help patients whose cancers do not respond,” said study co-leader Giorgio Trinchieri, MD, chief of the Laboratory of Integrative Cancer Immunology in NCI’s Center for Cancer Research. “Our study is one of the first to demonstrate in patients that altering the composition of the gut microbiome can improve the response to immunotherapy. The data provide proof of concept that the gut microbiome can be a therapeutic target in cancer.”
Trinchieri and colleagues report on their trial results in a paper titled, “Fecal microbiota transplant overcomes resistance to anti-PD-1 therapy in melanoma patients.”
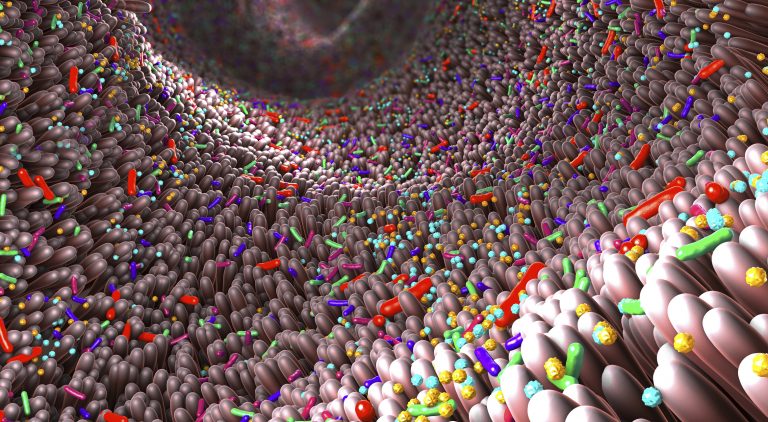
Immune checkpoint blockade using monoclonal antibodies (mAbs) targeting programmed cell death protein 1 (PD-1) provides long-term clinical benefits to nearly 40% of patients with advanced melanoma, the authors wrote. Research suggests that communities of bacteria and viruses in the intestines can affect the immune system and its response to chemotherapy and immunotherapy, including anti-PD-1 therapy. Interestingly, they continued, “the composition of the gut microbiota correlates with anti–PD-1 efficacy in preclinical models and cancer patients.” And previous studies have shown that tumor-bearing mice that do not respond to immunotherapy drugs can start to respond if they receive certain gut microorganisms from mice that responded to the drugs. However, there are still questions, the team acknowledged. “Although multiple studies have reported that a favorable gut microbiome is associated with response to anti–PD-1 in cancer patients, its precise composition is not yet fully understood.”
More research is needed, Trinchieri added, to identify the specific microorganisms that are critical for overcoming a tumor’s resistance to immunotherapy drugs and to investigate the biological mechanisms involved. Changing the gut microbiome may “reprogram” the microenvironments of tumors that resist immunotherapy drugs, making them more favorable to treatment with these medicines, he suggested.
“FMT is just a means to an end,” further explained study co-lead author Diwakar Davar, MD, a medical oncologist and member of the Cancer Immunology and Immunotherapy Program (CIIP) at UPMC Hillman and assistant professor of medicine at the University of Pittsburgh School of Medicine. “We know the composition of the intestinal microbiome – gut bacteria – can change the likelihood of responding to immunotherapy. But what are ‘good’ bacteria? There are about 100 trillion gut bacteria, and 200 times more bacterial genes in an individual’s microbiome than in all of their cells put together.”
To test whether fecal transplants are safe and may help patients with cancer better respond to immunotherapy, Trinchieri and colleagues developed a small, single-arm clinical trial for patients with advanced melanoma. The patients’ tumors had not responded to one or more rounds of treatment with the immune checkpoint inhibitors pembrolizumab (Keytruda) or nivolumab (Opdivo), which were administered alone or in combination with other drugs. Immune checkpoint inhibitors release a brake that keeps the immune system from attacking tumor cells.
In the study, the fecal transplants, which were obtained from patients with advanced melanoma who had responded to pembrolizumab, were analyzed to ensure that no infectious agents would be transmitted. After treatment with saline and other solutions, the fecal transplants were delivered to the colons of patients through colonoscopies, and each patient also received pembrolizumab.
After these treatments, 6 out of 15 patients who had not originally responded to pembrolizumab or nivolumab responded with either tumor reduction or long-term disease stabilization. One of these patients has exhibited an ongoing partial response after more than two years and is still being followed by researchers, while four other patients are still receiving treatment and have shown no disease progression for over a year.
The treatment was well tolerated, though some of the patients experienced minor side effects that were associated with pembrolizumab, including fatigue. “FMT shifted microbiome composition toward taxa favoring anti–PD-1 efficacy to induce clinical responses to anti–PD-1 in PD-1–refractory melanoma patients, who had an immunological ability to respond to the treatment but exhibited an unfavorable microbiota composition,” the team noted.
“The likelihood that the patients treated in this trial would spontaneously respond to a second administration of anti-PD-1 immunotherapy is very low,” said study co-senior author Hassane Zarour, MD, a cancer immunologist and co-leader of the CIIP at UPMC Hillman as well as a professor of medicine at Pitt. “So, any positive response should be attributable to the administration of fecal transplant.”
The NCI team analyzed microbiome samples from these patients to understand why FMT seems to boost their response to immunotherapy. The six patients whose cancers had stabilized or improved showed increased numbers of bacteria that have been associated with the activation of immune cells called T cells and with responses to immune checkpoint inhibitors.
In addition, by analyzing data on proteins and metabolites in the body, the researchers observed biological changes in patients who responded to the transplant. For example, levels of immune system molecules that are associated with resistance to immunotherapy declined, and levels of biomarkers that are associated with response increased. “Responders had distinct proteomic and metabolomic signatures, and transkingdom network analyses confirmed that the gut microbiome regulated these changes,” the scientists said.
Commenting on their results, the investigators further stated, “Collectively, our findings show that FMT and anti–PD-1 changed the gut microbiome and reprogrammed the tumor microenvironment to overcome resistance to anti–PD-1 in a subset of PD-1 advanced melanoma … Responders exhibited increased abundance of taxa that were previously shown to be associated with response to anti–PD-1, increased CD8+ T cell activation, and decreased frequency of interleukin-8–expressing myeloid cells.”
Based on the study findings, the researchers suggested that that future clinical trials should be conducted to confirm the results and identify biological markers that could eventually be used to select patients who are most likely to benefit from treatments that alter the gut microbiome. Davar and Zarour hope to run a larger trial with melanoma patients, as well as evaluate whether FMT may be effective in treating other cancers. Ultimately, the goal is to replace FMT with pills containing a cocktail of the most beneficial microbes for boosting immunotherapy, although that potential is still several years away.
“Even if much work remains to be done, our study raises hope for microbiome-based therapies of cancers,” said Zarour, who holds the James W. and Frances G. McGlothlin Chair in Melanoma Immunotherapy Research at UPMC Hillman.
“We expect that future studies will identify which groups of bacteria in the gut are capable of converting patients who do not respond to immunotherapy drugs into patients who do respond,” added study co-first author, Amiran Dzutsev, MD, PhD, of NCI’s Center for Cancer Research. “These could come from patients who have responded or from healthy donors. If researchers can identify which microorganisms are critical for the response to immunotherapy, then it may be possible to deliver these organisms directly to patients who need them, without requiring a fecal transplant.”













