A team of researchers, led by bioengineers at the Georgia Institute of Technology, has shown that modifying CAR T-cell therapies improves the precision and capabilities of these therapies to be used against solid tumors. The research—published recently in Nature Biomedical Engineering has the potential to broaden the reach of CAR T-cell therapies and significantly impact cancer treatment.
CAR T-cell therapy involves engineering a patient’s T cells, a type of white blood cell, in a lab. Then a chimeric antigen receptor (CAR) is added, and these customized immune cells are returned to the patient’s body, where they seek and destroy cancer cells. That’s how it works when it works.
“These therapies have proven to be remarkably effective for patients with liquid tumors— so, tumors that are circulating in the blood, such as leukemia,” explained senior study investigator Gabe Kwong, Ph.D., associate professor in the Wallace H. Coulter department of biomedical engineering at Georgia Tech and Emory. “Unfortunately, for solid tumors—sarcomas, carcinomas—they don’t work well. There are many different reasons why. One huge problem is that the CAR T-cells are immunosuppressed by the tumor microenvironment.”
Kwong and his collaborators are changing the environment and making some cell modifications of their own to enhance the way CAR T-cells fight cancer. They’ve added a genetic on-off switch to the cells and developed a remote-control system that sends the modified T cells on a precision invasion of the tumor microenvironment, where they kill the tumor and prevent a relapse.
The latest study builds on the lab’s body of work exploring remotely controlled cell therapies, in which the researchers can precisely target tumors, wherever they are in the body, with a local deposition of heat. “And this heat basically activates the CAR T-cells inside the tumors, overcoming the problems of immunosuppression,” Kwong noted.
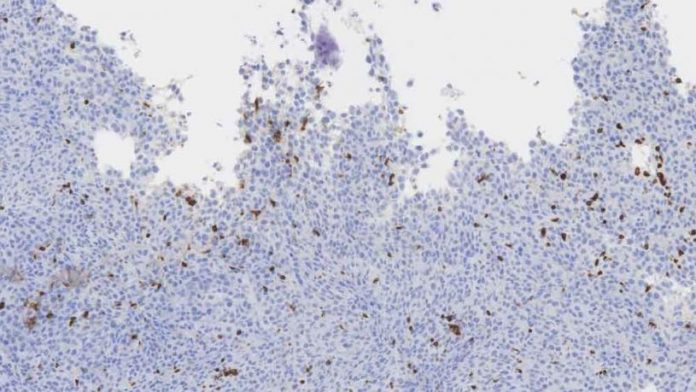
In the earlier study, the researchers did not clinically treat tumors, but they are doing that now with the new work. To generate heat in a mouse’s tumor, they shone laser pulses from outside the animal’s body onto the spot where a tumor is located. Gold nanorods delivered to the tumor turn the light waves into localized, mild heat, raising the temperature to 40–42 °C (104–107.6 °F), just enough to activate the T cells’ on-switch, but not so hot that it would damage healthy tissue or the T cells. Once turned on, the cells go to work, increasing the expression of cancer-fighting proteins.
The real novelty, Kwong said, was in genetically engineering clinical-grade CAR T-cells, something the team worked on for the past three years. Now, in addition to a switch that responds to heat, the researchers have added a few upgrades to the T cells, rewiring them to produce molecules to stimulate the immune system.
Localized production of these potent, engineered proteins (cytokines and bispecific T-cell engagers) has to be controlled precisely.
“These cancer-fighting proteins are really good at stimulating CAR T-cells, but they are too toxic to be used outside of tumors,” said Kwong. “They are too toxic to be delivered systemically. But with our approach, we can localize these proteins safely. We get all the benefits without the drawbacks.”
The latest study shows the system cured cancer in mice, and the team’s approach not only shrunk tumors but prevented relapse—critical for long-term survival. Further studies will delve into the additional tailoring of T cells and how the heat will be deposited at the tumor site. A gentle laser was used to heat the tumor site. That won’t be the case when the technology moves on to human studies.
“We showed that the activity of intratumoral CAR T-cells could be controlled photothermally via synthetic gene switches that trigger the expression of transgenes in response to mild temperature elevations (to 40–42 °C),” the authors wrote. “In vitro, heating engineered primary human T cells for 15–30 min led to over 60-fold-higher expression of a reporter transgene without affecting the cells’ proliferation, migration, and cytotoxicity. In mice, CAR T-cells photothermally heated via gold nanorods produced a transgene only within the tumors.”
“We’ll use focused ultrasound, which is completely noninvasive and can target any site in the body,” Kwong concluded. “One of the limitations with laser is that it doesn’t penetrate very far in the body. So, if you have a deep-seated malignant tumor, that would be a problem. We want to eliminate problems.”













