Scientists in Cambridge, England announced that they have created a new tool for predicting an individual’s risk of developing prostate cancer, one that could improve testing accuracy and reduce unnecessary and potentially invasive testing for men at low risk.
Developed by a team from the University of Cambridge and The Institute of Cancer Research, London, the tool, called CanRisk-Prostate, will be incorporated into the group’s existing CanRisk web tool, which has now recorded almost 1.2 million risk predictions in exsiting releases assessing risk for the development of breast and ovarian cancers.
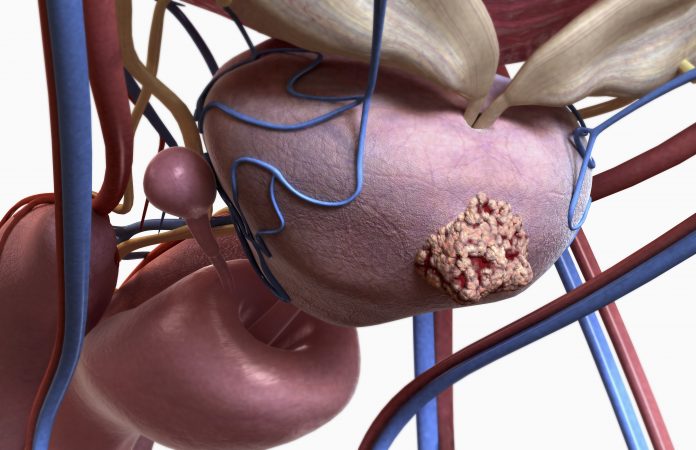
Testing for prostate cancer involves a blood test that looks for a protein known as a prostate-specific antigen (PSA) that is made only by the prostate gland; however, it is not always accurate. According to England’s National Health Service (NHS) website, roughly three quarters of men with a raised PSA level will not have cancer. For this reason, follow up testing such as tissue biopsies or MRI scans, are required to confirm a diagnosis.
“Population-wide screening based on PSA isn’t an option: these tests are often falsely positive, which means that many men would then be biopsied unnecessarily,” said Prof. Antonis Antoniou from the Department of Public Health and Primary Care at the University of Cambridge. “Also, many prostate tumors identified by PSA tests are slow-growing and would not have been life-threatening. The treatment of these tumors may do more harm than good.
“What we need is a way of identifying those men who are at greatest risk, allowing us to target screening and diagnostic tests where they are most needed, while also reducing the harms for those men who have low risk of the disease. This is what CanRisk-Prostate aims to do. For the first time, it combines information on the genetic makeup and prostate cancer family history, the main risk factors for the disease, to provide personalized cancer risks.”
Prostate cancer is one of the most genetically determined of common cancers. Inherited faulty versions of the BRCA2, HOXB13 and possibly BRCA1 genes are associated with moderate-to-high risk of prostate cancer, though such faults are rare in the population. In addition, there are several hundred more common genetic variants that each confer a lower risk, but in aggregate they act like ‘volume control’ that moderate or increase the prostate cancer risk.
The researchers describe the development of the first comprehensive prostate cancer model using genetic and cancer family history data from almost 17,000 families affected by prostate cancer in The Journal of Clinical Oncology. It employs data on rare genetic faults in moderate-to-high-risk genes and produces a polygenic risk score based on 268 common low-risk variants, together with detailed cancer family history, to predict the future risks.
One in six men (16%) will develop prostate cancer by the time they are 85 years old. Using the model, the team found that the predicted risk was higher for men who had a father diagnosed with prostate cancer—27% if the father was diagnosed at an older age (80 years) but as high as 42% if the father was diagnosed at a young age (50 years).
In practice, say the researchers, clinicians will be able to use any combination of cancer family history, rare and common genetic variants to determine personalized risk.
To validate their model, the team ran the risk model on an independent cohort of over 170,000 men recruited to UK Biobank. All of the men were free from prostate cancer when they were recruited to the study, but more than 7,600 developed prostate cancer within the subsequent ten years.
During validation of the model, the researchers found that 86% of the UK Biobank participants who developed cancer were in the half of men with the highest predicted risks—suggesting the possibility of targeting screening and diagnostic tests to the subgroup of the population at highest risk.
Prof. Ros Eeles from The Institute of Cancer Research, London and co-author on the study said: “This is an important step forward as it will enable clinicians to have conversations with men about their individual risk of prostate cancer based on the most accurate computer model to date. This will help them in making decisions about screening.”
So far, the data used to develop CanRisk-Prostate has been from men of European ancestry. The team hope to be able to include data from men of other ethnicities as further research is undertaken.













