University of Pittsburgh researchers have detailed how probiotic bacteria travel from the gut to cancer tumors and then stimulate immune cells to make melanoma immunotherapy more effective. The team showed that Lactobacillu reuteri, a lactic acid bacterium and known probiotic, stimulates cancer-killing T cells to secrete the compound idole-3-aldehyde (I3A). In a mouse study, the team gave the mice a diet rich in the amino acid tryptophan, which the bacteria converted to I3A, and found that immunotherapy drugs had a more pronounced effect in restraining tumor size and prolonging survival.
“We knew that gut microbes influence immunotherapy response, but there were still big questions about how they do this and whether they act from the gut or if they have to be at the tumor site,” said Marlies Meisel, PhD, assistant professor in the Department of Immunology at Pitt’s School of Medicine and the study’s senior author. “Our study is the first to show that orally administered bacteria increase efficacy of cancer immunotherapy by moving to tumors outside of the gut where they directly impact immune cells in the tumor.”
The gut microbiome has been a central focus of studies to better understand why immunotherapies are effective for some people and not others. And research has shown a link between taking probiotic supplements and immunotherapy response in melanoma patients.
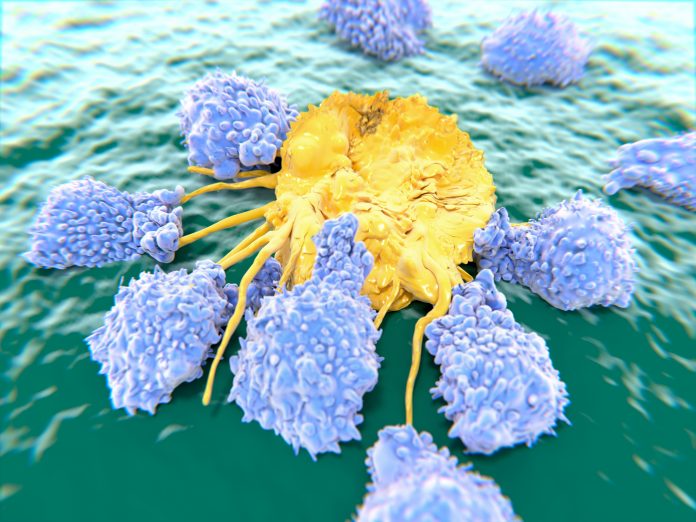
For their research, the results of which were published this week in the journal Cell, Meisel and colleagues fed L. reuteri, a bacterium that is often available in probiotics, to germ-free mice with melanoma. The team was able to demonstrate that the bacteria moved from the gut to the tumors where they established and persisted over time. Comparing these mice to a control group showed that those that received L. reuteri, had greater quantities of CD8 T cells—known as killer T cells—at the tumor site, that the tumors shrank more, and the mice lived longer.
The researchers further showed this effect was not particular to melanoma. Similar work in mouse models of adenocarcinoma, fibrosarcoma, and breast cancers, showed similar activity of the bacteria moving from the gut to the tumor and suppressing tumor growth.
Having seen this effect, the University of Pittsburgh researchers delved deeper to understand the mechanism by which L. reuteri helped amplify immunity. They discovered that the bacterium producing I3A activates a receptor on the CD8 cells that enhance their cancer-killing properties. Removing the receptor on the CD8 cells eliminated the ability of L. reuteri to induce anti-tumor immunity, showing that the effect was dependent on the CD8 receptor. Further, the researchers studied the effects of a genetically modified strain of L. reuteri that can’t produce I3A and found that the compound is essential to produce the anti-tumor activity.
“While the microbiome of tumors beyond the gut, including melanoma, had been described, the concept that tumor microbes play an active role in mediating cancer immunotherapy efficacy had not been demonstrated,” said Meisel. “So, we were surprised to find that I3A released by L. reuteri within the tumor enhanced immunotherapy response whereas the presence of L. reuteri in the gut was insufficient to have an anti-tumor effect.”
The next step was to determine whether what had been observed in the mouse models would also work to affect human response to immunotherapy. Analyzing blood samples from melanoma patients undergoing immune checkpoint inhibitor treatment, the researchers found that patients who responded well to immunotherapy had elevated I3A levels. Higher levels of I3A before treatment were also associated with a better chance of survival.
“Building on these findings in the future, it might be possible to use I3A levels as a biomarker to predict which patients are likely to respond to immunotherapy,” said Meisel. “Another direction I’m excited about is developing clinical trials to evaluate whether combining I3A with immunotherapy could improve outcomes for patients.”






![AI Algorithm Could Reduce Breast Cancer Mammogram False Positive Rate The primary goal of the Paradigm Registry is to accelerate tumor profiling based on disease biology. [iStock/LilliDay]](https://www.insideprecisionmedicine.com/wp-content/uploads/2019/01/307-218x150.jpeg)






