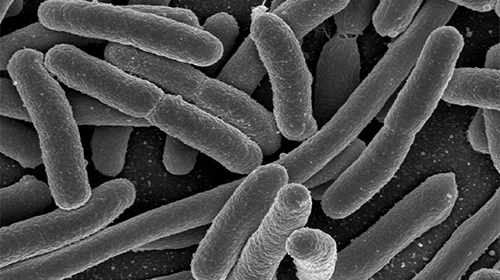
A large study analyzing genomic changes and antibiotic resistance in Escherichia coli bacteria across Norway shows patterns of emerging resistance over the last two decades and shows antibiotic resistance genes are being transferred across strains.
The study was carried out by researchers from the Wellcome Sanger Institute in the U.K. and the University of Oslo and compared the Norwegian findings with those from a similar study in the U.K. They showed that resistant strains started to emerge and increase in numbers in the early 2000’s, but that this resistance then increased more rapidly in the UK.
“The high number of samples from the Norwegian population and the level of genomic detail on the strains of bacteria enabled us to make much more far-reaching conclusions than were ever possible before,” said Jukka Corander, Ph.D., a professor at the University of Oslo and an associate faculty member at the Sanger, who co-led the research.
“This study demonstrates the power arising from a systematic national surveillance of resistant organisms, which both collects and makes the data available for in-depth analyses. Without these in place, it would have been impossible to approach the central research questions formulated in the study and find answers to them.”
E.coli is present in everyone’s gut as a harmless commensal bacterium, but it can become pathogenic and is responsible for a large number of bloodstream infections each year. Resistance to available antibiotics is increasing making these infections harder to treat. Knowing more about how such bacteria spread and reproduce can help public health authorities and clinicians develop better treatments and strategies to prevent further resistance.
This study included 22,512 samples collected from people with resistant E. coli bloodstream infections in Norway between 2002 and 2017. Whole genome sequencing of the bacteria in the samples was used to determine population structure. The results were then compared to a similar study carried out on UK samples collected between 2001 and 2011.
As reported in The Lancet Microbe journal, there was an increase of multidrug resistant CC131 isolates from 5.6% of samples tested in the 2002-2010 period to 10.5% of those tested between 2011-2017. However, the researchers note that the continued strong presence of non-resistant strains during this time suggests this genetic variant is not needed for survival.
Specifically within CC131 samples, the genetics changed over time with clade A increasing in this group from 2002, but the global multidrug resistant clade C2 not bring seen until 2007. CC131 clade A increased more rapidly in Norwegian samples than clade C2 and was more prevalent than in the UK at 27% versus 5.4% in this strain.
It took around 11 years for CC131 strains to become established in Norway versus approximately 2 years in the UK, although both countries had strongly established multidrug resistant strains by the end of the study sampling time.
“Even in a low antibiotic use setting, resistance to important antimicrobial classes has rapidly been selected for in a previously susceptible clade. This highlights the importance of future genomic surveillance in uncovering the complex ecology underlying multidrug resistance dissemination and competition, to support the design of strategies and interventions to control the spread of high-risk multidrug resistant clones,” write the researchers.
They caution that “clones and clades can differ significantly between European countries that are resource similar, highlighting the need for country-specific intensified surveillance efforts to circumvent the threat posed by the current evolutionary trajectory of E. coli causing bloodstream infections.”






![AI Algorithm Could Reduce Breast Cancer Mammogram False Positive Rate The primary goal of the Paradigm Registry is to accelerate tumor profiling based on disease biology. [iStock/LilliDay]](https://www.insideprecisionmedicine.com/wp-content/uploads/2019/01/307-218x150.jpeg)




