Researchers at Institute for Systems Biology (ISB) have developed a method using using single-cell analysis to measure metabolic activities in rare disseminated tumor cells taken from non-small cell lung cancer (NSCLC) patients that can accurately predict how patients will respond to various cancer therapies, and how treatments will impact a patient’s physiological performance and survival according to a study published in Nature Communications.
The study also demonstrated how the researchers pinpointed the molecular basis underlying these metabolic states. Importantly, it also identified potential treatment strategies for lung cancer patients who the test showed would be unlikely to respond well to standard chemotherapies or targeted therapies.
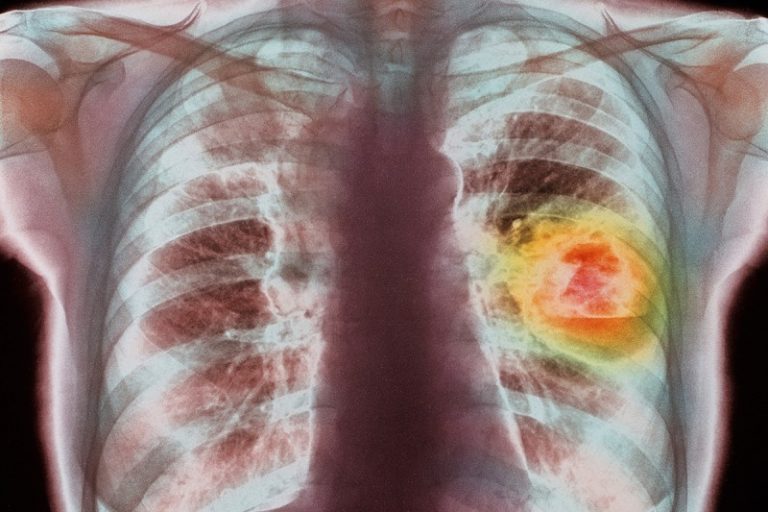
Advanced-stage NSCLC is a common and highly lethal form of cancer. Currently, there is no simple and cost-effective clinical method to predict NSCLC patient response before therapy starts or to identify potential drug resistance when patients are still benefiting from therapy.
“Our metabolic assay can provide unique information complementary to tumor genetics and other clinical factors for improved cancer diagnostics. For example, tumor genetics can identify whether the patients are bearing targetable driver oncogene mutations and thus segregate patients into various chemo- and targeted therapy regimens,” said Dr. Wei Wei, assistant professor at ISB and a corresponding author on the paper in a press release. “Our metabolic assay can further reveal whether patients are likely—or unlikely—to benefit from the standard chemotherapies or targeted therapies identified by tumor genetics. This is important particularly for newly diagnosed patients who may benefit from such predictions prior to the onset of therapy.”
According to the authors, the newly developed single-cell assay has the potential to be broadly adopted as it uses fluorescence imaging systems that are commonly found in hospitals’ clinical and cytopathology labs. It has the potential, they say, to provide oncologists with complementary information that can be used in conjunction with other testing results to improve clinical decision making and potentially shorten the time from diagnosis to a patient getting a highly targeted treatment selected specifically for their disease.
“The notion of precision cancer medicine has been mostly driven by tumor genomics. Except for PET imaging, functional assays are rarely used as diagnostic tools for clinical decision-making,” Wei said. “Our results highlight the promise of using cellular metabolic functions to address some of the most challenging questions in cancer diagnostics, namely predicting the diverse therapy responses for patients with similar tumor genetics in order to match the right patient with the right therapy.”
The researchers are now validating these findings in a larger patient cohort to set the stage for translation into the clinical setting.
The research by Dr. Wei Wei’s lab at ISB in collaboration with Dr. Qihui Shi’s lab at Fudan University, and Dr. Shun Lu’s lab at Shanghai Chest Hospital, Shanghai Jiao Tong University. Other major contributors include the Department of Molecular and Medical Pharmacology at UCLA’s David Geffen School of Medicine, and the Department of Chemistry at UC Riverside.













