Research from an international collaboration shows that a single-cell omics approach can identify mutational status and characterize gene expression in hematopoietic stem cells from acute myeloid leukemia patients and successfully identify disease causing cells.
Treatments exist for acute myeloid leukemia (AML), but while these often succeed initially, patients often relapse. Indeed, less than 15% of patients over the age of 60 survive for 5 years after treatment for this reason.
“Only cancer stem cells, residing at the top of the hierarchy, are able to fuel long-term cancer growth and drive relapse, whereas the bulk of the cancer consists of rapidly dividing cells with limited capacity for self-renewal,” write the researchers in the journal article describing the study in Nature Genetics.
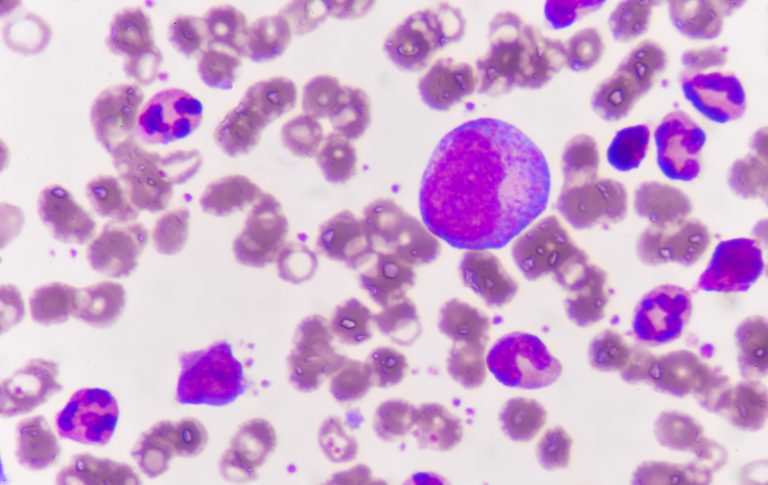
The problem in AML is that leukemic stem cells or pre-leukemic stem cells are present in small numbers and are hard to identify using conventional techniques so they often ‘hide’ in the system only to re-emerge as a cancer relapse months or years after treatment. This can make it hard to know which cells in the blood to destroy to truly eradicate the cancer without causing unnecessary damage to healthy cells.
To try and create a more effective system for identifying leukemic stem cells so they can be targeted, a research group including scientists at the Centre for Genomic Regulation in Barcelona, the European Molecular Biology Laboratory in Heidelberg, Heidelberg Institute for Stem Cell Technology and Experimental Medicine and Stanford University, among others, carried out a study using single cell transcriptomics and sequencing methods.
The team set up a workflow called MutaSeq, that enables researchers to assess mutational status of each blood cell and also assess gene expression. As reported in the journal Nature Genetics, they tested the system using samples from 4 patients with AML. They found they were able to differentiate between healthy hematopoietic stem cells and pre-leukemic or leukemic stem cells by looking at how different mutations impact gene expression in the cells.
They also gained insight into how many cells in the patients were leukemic and pre-leukemic stem cells, as opposed to healthy stem cells by using the mitoClone computational pipeline to track their accumulation.
The research team hope these results will help cancerous cells to be targeted better in these patients. “There are a huge number of small molecule drugs out there with demonstrated clinical safety, but deciding which cancers and more specifically which patients these drugs are well suited for is a daunting task,” says Lars Steinmetz, Ph.D., a professor at Stanford University, Group Leader at EMBL Heidelberg, and senior author of the paper.
“Our method can identify drug targets that might not have been tested in the right context. These tests will need to be carried out in controlled clinical studies, but knowing what to try is an important first step.”
As a next step, the scientists are planning to test their workflow in more patients and make it more streamlined. “Our vision is to identify cancer stem cell specific drug targets in a personalized manner, making it ultimately as easy for patients and doctors to look for these treatments as it is testing for coronavirus,” concludes lead author Lars Velten, Ph.D., a group leader at the Centre for Genomic Regulation and first author on the paper.











