The mechanism by which an inherited mutation causes the rare eye disease late-onset retinal degeneration (L-ORD) was revealed by researchers based at the National Eye Institute, part of the National Institutes of Health.
The research team, led by Kapil Bharti, who directs the Ocular and Stem Cell Translational Research Section of the institute, also identified two possible treatment approaches for this condition –one involving gene therapy, and the other the use of the well-known type 2 diabetes drug metformin.
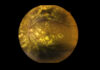
L-ORD is a rare type of eye disease that is inherited in a dominant fashion and caused by a missense substitution mutation in the gene CTRP5. A characteristic of the condition is the presence of thick, fatty deposits between the surface of the retina and Bruch’s membrane. Symptoms often don’t appear until midlife (40-60 years) and start by loss of vision in the dark and eventually lead to blindness.
As described in the journal Communications Biology, the researchers created a laboratory model of the disease by inducing pluripotent stem cells from the skin (fibroblasts) to make retinal pigment epithelium (RPE). One model was made using cells extracted from two siblings with L-ORD and another from cells from unaffected relatives as a control.
In the cells from patients with L-ORD, the researchers observed that the CTRP5 gene variant led to less CTRP5 protein being secreted. The cells were also deformed.
“The 5′ AMP-activated protein kinase (AMPK) has been suggested as an intracellular mediator of CTRP5 to regulate fatty acid metabolism and energy homeostasis,” write the authors. This was confirmed in this study.
The CTRP5 protein normally binds to adiponectin receptor 1 (ADIPOR1), which in turn impacts AMPK. With less CTRP5 binding to ADIPOR1, there is sustained activation of AMPK resulting in defective lipid metabolism, lower mitochondrial respiration, and reduced ATP production, among other factors, in the affected tissue.
The researchers also tested two possible treatments for L-ORD on the models, both of which effectively reduced signs of disease such as the fatty deposits on the RPE. The first was a gene therapy that was designed to improve expression of the CTRP5 protein and the other was treatment with metformin, which is known to regulate AMPK activity.
“Importantly, we now have two potential strategies to disrupt the L-ORD disease process. While gene therapy may be years away, metformin is a drug that’s long been used to treat diabetes,” said Bharti, who is planning with colleagues to test metformin therapy for treatment of L-ORD in a clinical trial.
Although L-ORD is rare, there are a number of more common diseases that also affect the RPE such as age-related macular degeneration and the team is planning to explore using their model to help investigate and treat these as well.
“This new model of a rare eye disease is a terrific example of translational research, where collaboration among clinical and laboratory researchers advances knowledge not by small steps, but by leaps and bounds,” said Michael Chiang, director of the National Eye Institute.