Researchers at the University of Edinburgh have discovered that early use of antibiotics in newborns can cause harm to the microbiome, potentially resulting in an adverse impact on later health, so they advise caution when prescribing these drugs to young babies.
In a study of 227 babies in their first week of life, the team also showed that certain types of antibiotics had a worse impact on beneficial gut microbes than others and suggest this should be taken into account if treatment for infection is needed.
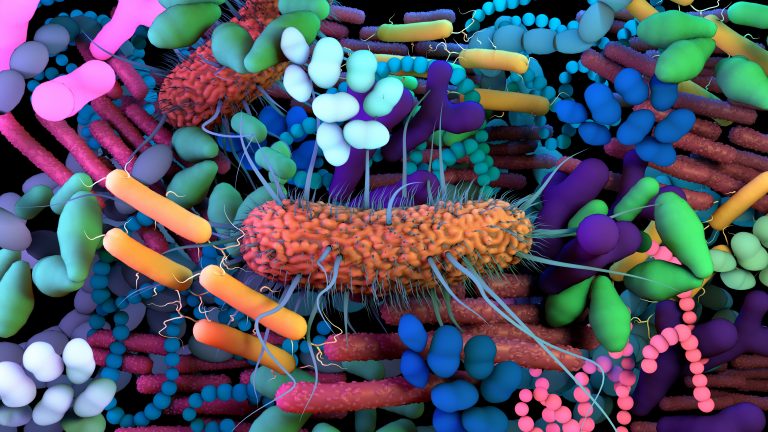
It is known that the first week of life is a critical time for microbiome formation in infants who obtain the first microbes of their gut microbiome during birth from their mothers. We still don’t know all the implications of healthy versus unhealthy gut microbiome formation, but it can help with food digestion and the development of a healthy immune system, among many other factors.
Due to suspected early-onset neonatal sepsis, as many as 10% of newborn babies are given broad-spectrum antibiotics as treatment, even though many are not actually infected and are treated quickly due to the speed that sepsis can spread.
The impact of these drugs on the microbiome of these babies and their overall health has not been studied intensively. To remedy this and to assess if some antibiotic combinations are better than others for these children, study lead Debby Bogaert, Chair of Pediatric Medicine at the University of Edinburgh, who is also affiliated with the University Medical Center Utrecht, and colleagues carried out a study where they compared the microbiome of newborns given different antibiotic combinations for suspected sepsis with healthy controls.
Overall, 147 newborn infants with suspected sepsis were randomly assigned (1:1:1) to receive three different antibiotic combinations—penicillin + gentamicin, co-amoxiclav + gentamicin or amoxicillin + cefotaxime over 48 hours on average. A group of 80 healthy newborns served as controls.
As described in the journal Nature Communications, the team collected rectal swabs or feces to collect gut microbiome samples before and immediately after treatment, and also at one, four and 12 months of life. 16S rRNA-based sequencing was used to characterize the microbiome species and 31 antimicrobial resistance genes were also tested for using qPCR.
The team found that there was a big difference in the gut microbiomes of treated children versus controls straight after treatment that gradually normalized over 12 months. More specifically, the treated babies had lower levels of Bifidobacterium bacteria, which can help babies digest milk. There were also higher levels of the potentially disease causing Klebsiella and Enterococcus bacterial species in babies given antibiotics than in those who were not.
“We were surprised with the magnitude and duration of the effects of broad-spectrum antibiotics on the infants’ microbiome when compared to effects of those same antibiotics on adults’ microbiota. This is likely because the antibiotic treatment is given at a time that infants have just received their first microbes from their mother and have not yet developed a resilient microbiome,” said Bogaert in a press statement.
Of the three drug combinations, amoxicillin + cefotaxime had the most adverse effect on the infants microbiome and penicillin + gentamicin the least, with the latter linked with the emergence of less antimicrobial resistance genes.
Willem van Schaik, Professor of Microbiology and Infection at the University of Birmingham and study co-author, said: It is particularly troubling that following antibiotic therapy in newborns we observed a strong increase in Klebsiella and Enterococcus species which are both important multidrug-resistant pathogens.
“This underlines the importance of further studies into balancing the need and effectiveness of these antibiotics and the risk of the emergence of genes linked with resistance. There may also be scope to develop new interventions, like live biotherapeutics—a treatment that is produced by or involving living cells—to effectively restore the composition of the infant gut microbiome after antibiotic therapy.”













