Pharmaceutical company Agios has received FDA approval for its acute myeloid leukemia (AML) drug Tibsovo (ivosidenib) tablets for the treatment of adult patients with relapsed or refractory acute myeloid leukemia (AML) who have specific mutations in the IDH1 gene as identified by a companion diagnostic.
“Tibsovo is a targeted therapy that fills an unmet need for patients with relapsed or refractory AML who have an IDH1 mutation,” said Richard Pazdur, M.D., director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research in a press release. “The use of Tibsovo is associated with a complete remission in some patients and a reduction in the need for both red cell and platelet transfusions.”
Agios first submitted its application for ivosidenib for the (AML) indication in late December last year with a request for priority review. The FDA granted the application Fast Track and Priority Review designations. It also received Orphan Drug designation, which provides incentives to assist and encourage the development of drugs for rare diseases.
“People with AML who have relapsed or refractory disease have limited treatment options available to them, and it is our hope that we can change that,” Chris Bowden, M.D., CMO of Agios said last December. “Earlier this month at the ASH Annual Meeting, we presented compelling single agent ivosidenib data demonstrating durable responses in high-risk relapsed or refractory AML patients with an IDH1 mutation. These data highlight the potential for ivosidenib to be a first-in-class therapy for patients with R/R AML and an IDH1 mutation.”
According to the Leukemia & Lymphoma Society (LLS), the approval of ivosidenib comes amid a flurry of approvals in the past two years, after a 40-year drought of new treatments for AML. Three of the approvals, including ivosidenib and its sister IDH2 inhibitor, enasidenib, are first-time approvals, while the others are for new formulations, new indications, or reinstatement of agents that has received approval previously.
The lack of approvals in the past 40 years has largely been due to a lack of a more precise understanding of AML. Advances in molecular analysis has allowed for a greater understanding of the specific genetic mutations characteristic of AML and have provided provided targets, such as IDH1, for the development of new drugs.
“For so long, AML patients have desperately needed new and better options for treatment,” said Louis J. DeGennaro, LLS President and CEO. “And for too long, AML has been treated as a one-size-fits-all disease, so it is encouraging to see these new treatments added to the armamentarium for AML patients. Today's approval is further proof that we are headed in the right direction with a precision medicine approach to conquering this difficult cancer.”
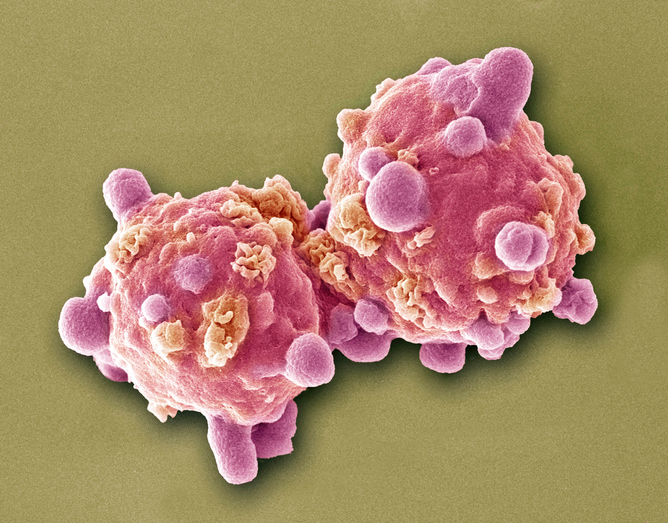
AML is a rapidly progressing cancer that forms in the bone marrow and results in an increased number of abnormal white blood cells in the bloodstream and bone marrow. The National Cancer Institute at the National Institutes of Health estimates that approximately 19,520 people will be diagnosed with AML this year; approximately 10,670 patients with AML will die of the disease in 2018.











