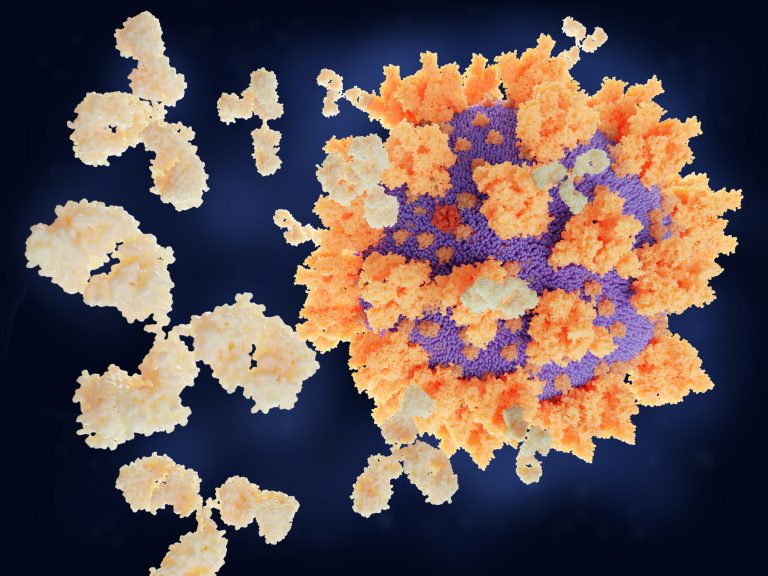
Developing a better understanding surrounding both T cell and B cell response to the SARS-Cov-2 infection, and the amount of time each remains active, is an important factor to implement strategies to combat the pandemic. Now, two separate studies suggest that antibodies against SARS-CoV-2 can last at least three months after a person becomes infected with the virus.
Published together in Science Immunology, the studies have documented the persistence of antibodies that target SARS-CoV-2 in hundreds of patients with COVID-19 at least three months after symptom onset. Both studies point to the IgG class of antibodies as the longest-lasting antibodies detectable in the blood and saliva of patients during this timeframe, suggesting that SARS-CoV-2-specific IgG antibodies may serve as promising targets to detect and evaluate immune responses against the virus.
One group’s work is published in a paper titled, “Persistence of serum and saliva antibody responses to SARS-CoV-2 spike antigens in COVID-19 patients.”
Researchers used saliva and blood samples from COVID-19 patients to measure and compare antibody levels for over three months post-symptom onset. They found that IgG antibodies that bind to the SARS-CoV-2 spike protein are detectable for at least 115 days, representing the longest time interval measured. The study is also the first to show these antibodies can also be detected in the saliva.
The researchers found that while IgA and IgM antibodies targeting the spike protein’s receptor binding domain rapidly decayed, IgG antibodies remained relatively stable for up to 105 days after symptom onset in 402 patients with COVID-19. They charted the patients’ antibody responses from 3 to 115 days after symptom onset, and compared their profiles with 339 pre-pandemic controls. Patients with COVID-19 showed peak IgG levels at 16 to 30 days after the appearance of symptoms.
Levels of all spike protein-specific IgG, IgM, and IgA antibodies in the blood positively correlated with levels observed in matched saliva samples.
“Our study shows that IgG antibodies against the spike protein of the virus are relatively durable in both blood and saliva,” said Jennifer Gommerman, PhD, professor of immunology at the University of Toronto. “Our study suggests saliva may serve as an alternative for antibody testing. While saliva is not as sensitive as serum, it is easy to collect.”
While the team admits there is a lot they still don’t know about antibody responses to SARS-CoV-2 infection, including how long the antibodies last beyond this period or what protection they afford against re-infection, this research could have broader implications in the development of an effective vaccine.
“This study suggests that if a vaccine is properly designed, it has the potential to induce a durable antibody response that can help protect the vaccinated person against the virus that causes COVID-19,” Gommerman said.
The second study, led by a Boston group, is published in the paper titled, “Persistence and decay of human antibody responses to the receptor binding domain of SARS-CoV-2 spike protein in COVID-19 patients.”
The team measured antibody responses in the blood of 343 patients with COVID-19 for up to 122 days after symptom onset—and compared these responses to those of 1,548 control individuals sampled before the pandemic.
The researchers focused only on antibodies specific to the SARS-CoV-2 spike protein’s receptor binding domain. To provide a baseline, the researchers estimated sensitivities of IgG, IgA, and IgM antibody types at 95%, 90%, and 81%, respectively, for detecting infected individuals between 15 to 28 weeks after symptom onset. Among these antibodies, spike protein-specific IgM and IgA were short-lived, dropping beneath detection levels at around 49 and 71 days, respectively, after the appearance of symptoms. In contrast, spike protein-targeted IgG responses decayed slowly over a period of 90 days, with only three individuals losing them within this timeframe. Levels of spike protein-specific IgG strongly correlated with levels of neutralizing antibodies in the patients. The researchers also did not observe cross-reactivity of any SARS-CoV-2-targeting antibodies with other “common cold” coronaviruses.
IgG levels remained elevated in these patients for four months, and were associated with the presence of protective neutralizing antibodies, which also demonstrated little decrease in activity over time. “That means that people are very likely protected for that period of time,” said Richelle Charles, MD, an investigator in the division of infectious diseases at MGH. “We showed that key antibody responses to COVID-19 do persist.”
In another finding, Charles and her colleagues showed that people infected with SARS-CoV-2 had IgA and IgM responses that were relatively short-lived, declining to low levels within about two and a half months or less, on average. “We can say now that if a patient has IgA and IgM responses, they were likely infected with the virus within the last two months,” said Charles.
Knowing the duration of the immune response by IgA and IgM will help scientists obtain more accurate data about the spread of SARS-CoV-2, explained Jason Harris, MD, a pediatric infectious disease specialist at MGH and co-senior author of the study. “There are a lot of infections in the community that we do not pick up through PCR testing during acute infection, and this is especially true in areas where access to testing is limited,” he said. “Knowing how long antibody responses last is essential before we can use antibody testing to track the spread of COVID-19 and identify ‘hot spots’ of the disease.”