Semen could be considered a liquid biopsy of the organs of male reproductive system—specifically, of the prostate gland. This is convenient. Semen is, potentially, a source of prostate disease-specific molecules, which are of intense interest because they could lead to better diagnostic tests. If so, semen-based tests could augment or replace the serum prostate-specific antigen (PSA) screen. Although the PSA screen is credited with a significant decrease in deaths due to prostate cancer, it still has serious limitations.
At the Bellvitge Biomedical Research Institute (IDIBELL) and the Bellvitge University Hospital (HUB), researchers decided to evaluate semen as a source of prostate cancer biomarkers. The researchers, led by Sara Larriba, Ph.D., a principal investigator at IDIBELL, focused their search on extracellular miRNAs, which are present within the semen in extraordinary concentrations.
Importantly, some of these extracellular miRNAs are specific to the prostate gland. Also, according to previous research carried out by other scientists, distinct miRNA expression patterns occur in prostate tumor tissue, supporting the idea that miRNAs could serve as biomarkers for prostate cancer.
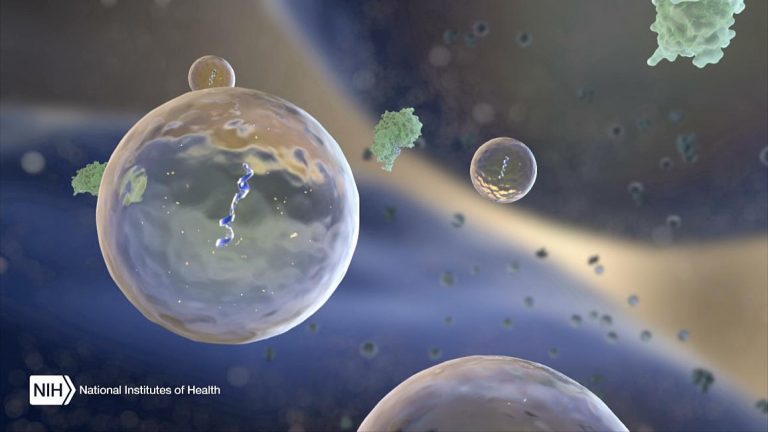
Encouraged by the evident potential of miRNAs in prostate cancer diagnostics, and hopeful that extracellular miRNAs could be as telling as tumor tissue miRNAs, Larriba and colleagues profiled the expression levels of the miRNAs contained in semen. Semen miRNAs may be carried within cell-derived extracellular vesicles, such as exosomes, or they may travel through semen freely or as a component of soluble protein complexes. The miRNAs in semen exosomes are presumably relatively well protected from degradation.
Larriba and colleagues profiled the expression level of miRNAs contained in semen exosomes from men with moderately increased PSA levels to assess their usefulness, either alone or in addition to PSA marker, as noninvasive biomarkers. This work allowed the scientists to uncover a distinctive miRNA expression pattern in exosomal semen samples taken from men with prostate cancer. The pattern, the scientists emphasized, is unlike that found in the exosomal semen samples taken from healthy men.
“We found that the levels of 50 miRNAs in exosomes were altered in prostate cancer (PCa) and benign prostatic hyperplasia (BPH) compared with healthy controls when assessed by miRNA qPCR arrays that profiled 634 human miRNAs,” wrote the article’s authors. “These results were validated for 14 miRNAs in a larger cohort of patients.
“Specifically three miRNAs (miR-142-3p, miR-142-5p, miR-223-3p) were confirmed as being at significantly higher levels in men with moderately elevated PSA levels and biopsy-proven cancer. The corresponding upregulation of these three miRNAs in PCa and BPH tissue suggest that the concentration of these miRNAs in SP exosomes can indeed reflect prostate health.”
According to Larriba, the current study suggests that semen exosome miRNA-based models as molecular biomarkers have the potential to improve prostate cancer diagnosis/prognosis efficiency. “These miRNA-based tests should provide reliable information that will help physicians make clinical decisions,” she said. “These tests could also help patients avoid unnecessary invasive biopsies, improving the efficiency of detection of prostate cancer and patient outcome.”
“In many cases, having elevated PSA levels does not mean having prostate cancer,” noted Francesc Vigués, a HUB researcher and a co-author of the current study. “Thus, PSA screening has resulted in an overdiagnosis of prostate cancer, and in many unnecessary biopsies of benign disease.”
“Serum PSA levels do not correlate with tumor aggressiveness, survival, or response to pharmacological treatments leading to over-treatment of indolent tumors,” added Manel Castells, another HUB researcher who contributed to the study. “Given this context, more accurate noninvasive biomarkers for prostate cancer with diagnostic and prognostic purposes would be very welcomed indeed.”
“Our aim,” Larriba pointed out, “is to offer our results to the clinics as a diagnostic test. In that respect, as our next step, we should carry out further prospective studies on larger cohorts of patients before this miRNA-based biomarker could be adopted in the daily clinical practice.”











