
Finding an effective treatment for Alzheimer’s disease has proved to be a long and difficult quest, but the approval of lecanemab (Leqembi®) last year for the treatment of early-stage disease was a pivotal turning point for the field.
Alzheimer’s is a disease associated with aging and impacts almost seven million people in the U.S. over the age of 65, with women and Black or Hispanic populations disproportionately affected by the condition. During the disease process of Alzheimer’s, amyloid beta protein misfolds to form amyloid plaques and tau protein forms what are known as neurofibrillary tangles in the brain.
The process of amyloid plaque formation can be split into different phases, starting with soluble amyloid beta oligomers that gather to form larger protofibrils. These are eventually converted into amyloid fibrils, which are deposited as plaques in the brain.
Although both amyloid and tau aggregation are now known to be part of Alzheimer’s disease pathology, the importance and toxicity of each part of the process is less clear. Different companies have decided to target different parts of the amyloid plaque and tau tangle formation process in the hope of stopping neurodegeneration in its tracks.
The so-called “amyloid hypothesis” came under much criticism during years of failed trials but has finally been backed up by the lecanemab results and approval as the drug targets amyloid protofibrils.
“I think it was a bit of a relief for the area … it’s the first time there were monoclonal antibodies against amyloid beta that actually showed statistically significant efficacy,” said Vandria CEO, Klaus Dugi, MD, in an interview. The Swiss biotech is taking a different approach to treating Alzheimer’s and other diseases by aiming to correct mitochondrial dysfunction, something that is significant in the brains of people with the condition.
Treatment options for Alzheimer’s have been very limited for a long time. For many years, the only real options were acetylcholinesterase inhibitors, such as tacrine and rivastigmine, and an NMDA receptor antagonist called memantine, none of which have a large impact on symptoms.
There are several reasons driving the difficulty in getting new treatments for Alzheimer’s to the market. “One is the lack of translation from rodent models to humans. There is an abundance of therapeutic approaches that have shown efficacy in mouse models of Alzheimer’s that eventually did not show the same efficacy in human trials,” Dugi told Inside Precision Medicine.
“The second challenge is that most of the Alzheimer’s trials will be of 12–18 months duration and will have between 500–1,500 patients. So, they’re very costly,” he added.
AC Immune, also based in Switzerland, was an early participant in the race to get new drugs to the market. Although the biotech company has good Alzheimer’s candidates in its pipeline, it has also experienced trial failures. For example, its monoclonal antibody crenezumab, designed to target amyloid beta, failed to show promising results in both Phase II and Phase III clinical trials.

CEO and founder, AC Immune
Company CEO and founder Andrea Pfeifer, PhD, believes her company and the field can more generally benefit from recent advances in Alzheimer’s and neurodegenerative biomarkers and diagnostic technology, and by taking a precision medicine approach to the field. “We just didn’t have the tools before. You couldn’t do precision medicine, you couldn’t do diagnostics in selected patients, but we do have them now,” she emphasized.
According to the ClinicalTrials.gov website, at the beginning of 2023, there were 187 trials in progress assessing the efficacy of 141 candidate therapies for Alzheimer’s. There is no doubt that the approval of lecanemab gave a huge boost to the field, both in terms of validating years of research, providing a better option for patients and increasing interest from investors. With a number of late-stage trial readouts due this year, it seems the field of Alzheimer’s therapeutics is finally on an upward trajectory.

Exploring antibody therapies
Lecanemab was developed by Biogen and Eisai in partnership with BioArctic. The Phase III trial that led to its full approval in July 2023 showed that it was able to slow cognitive decline in early-stage Alzheimer’s patients by a statistically significant 27% compared with placebo during an 18-month study.
Lecanemab is not the first monoclonal antibody to receive FDA approval for treatment of Alzheimer’s. In 2021, aducanumab (Aduhelm)—also developed by Biogen and Eisai—was granted accelerated (but not full) approval by the regulator. However, a cloud of controversy surrounded the decision because of concerns about changes to trial methodology, limited overall efficacy, and a high risk of side effects such as amyloid-related imaging abnormalities (ARIA), which can cause brain swelling in some people. While ARIA is also possible with lecanemab, the rates are much lower than those seen in patients treated with aducanumab.
Due largely to poor sales and the better efficacy and side effect profile of lecanemab, Biogen announced it would be stopping further development and sales of aducanumab in January and focusing its attention on the rest of its Alzheimer’s pipeline.
The next antibody treatment to be approved for treatment of Alzheimer’s disease will almost certainly be Eli Lilly’s therapy donanemab, which targets amyloid beta plaque. Lilly announced good Phase III results in May last year, published later that summer in JAMA, showing an overall 35% slowdown in disease-related cognitive decline compared with placebo in 1,736 individuals with early-stage, but symptomatic disease.

chief medical officer (CMO)
Acumen Pharmaceuticals
“It’s really nice to have these successes in the field,” said Eric Siemers, MD, chief medical officer (CMO) at Virginia-based biotech Acumen Pharmaceuticals, which is developing its own monoclonal antibody against amyloid oligomers.
“It’s great to go to meetings and have everybody be so upbeat, because after years of attacking the amyloid hypothesis … we finally are seeing these successes. Now, can we cure the disease? No, we’ve got a long ways to go. But at least we know we’re on the right track.”
Acumen also has an antibody therapy under development aimed at soluble amyloid beta oligomers, sabirnetug (ACU193). Following successful Phase I results, the company plans to start a Phase II/III study in the first half of this year.
“If you reduce plaque by enough, you seem to get some efficacy. But what the fields also learned over time is that the amyloid beta monomers and the insoluble fibrils that make up plaque are not really toxic, but there are toxic species called oligomers,” explained Siemers.
“If you put those oligomers on a neuron, you induce downstream pathologies, like tau phosphorylation. You cause a large increase in calcium influx into the cells, and you disrupt something called long-term potentiation, which is a normal physiologic function. The antibody that we’re testing ACU193 was designed to specifically bind to these oligomers.”
Acumen is banking on sabirnetug inducing a larger reduction in disease progression and a better side effect profile than lecanemab and donanemab. The Phase I results were promising, but whether this plays out in later stage trials remains to be seen.
Prothena Biosciences was spun out of Irish pharma company Élan Pharmaceuticals in 2012. Élan previously had a strong neurodegenerative disease focus and Prothena inherited much of its drug discovery pipeline from Élan.
Along with late-stage candidates for amyloidosis and Parkinson’s disease, Prothena has several Alzheimer’s disease candidates in development, including an anti-amyloid beta antibody (PRX012), an anti-MTBR-tau antibody (PRX005), both of which are in Phase I trials, and an amyloid beta and tau vaccine (PRX123) that has achieved investigational new drug (IND) clearance.
Prothena’s amyloid beta antibody differs from others in development because it can be given subcutaneously rather than by intravenous infusion.
“Prothena is developing a molecule that we certainly hope will be delivered at home, once monthly, by subcutaneous administration and can be self-administered. I think that from a treatment burden perspective that allows us to start to think about the idea that any patient should have access to these types of approaches, and we think that that’s very important,” said Gene Kinney, PhD, Prothena CEO and president.
“We did release actually a little bit of descriptive data in January from our very first multiple dose cohort of PRX012, where we did indicate that in addition to seeing biological activity that was encouraging, so reduction of amyloid as measured by non-invasive PET imaging and a permissive safety profile … we felt that the drug was amenable to once monthly dosing, so we were very excited about that.”
The company is also developing an anti-tau antibody in collaboration with Bristol-Myers Squibb. There has been a lot of debate about whether amyloid or tau protein aggregation is the best target for treating Alzheimer’s disease, but both are now thought to be important.
“In the early days, it was very much a discussion of is it amyloid beta or is it tau?” explained Kinney. “I think most of the field believes today that amyloid beta is probably the preceding event … it’s a key driver, to the subsequent things that are happening in Alzheimer’s disease, including tau dysregulation.”
Bringing genetics into the equation
To really bring a precision medicine approach to the world of Alzheimer’s therapeutics, it is important to consider genetics. Although Alzheimer’s is a multifactorial disease with different features contributing to its onset, certain genetic mutations or variants can increase or decrease a person’s risk of developing the condition.
For example, there are three major alleles of the apolipoprotein E (APOE) gene: E2, E3, and E4. E3 is the most common, with an estimated frequency around the world of 78%, whereas E2 and E4 are less common, with estimated worldwide frequencies of 8% and 14%, respectively. The E4 allele is linked to significantly increased risk for Alzheimer’s disease, particularly in homozygotes (2–3% population), who have two copies of the allele. In contrast, E2 carriers have significantly reduced risk of developing the condition.
APOE4 homozygotes appear to be at particular risk of ARIA if given anti-amyloid beta antibodies such as lecanemab and are therefore currently not eligible for these therapies. This makes them a group with a particularly high unmet treatment need, given their up to 15-fold increased risk of developing Alzheimer’s over the general population.

chief of staff, Alzheon
Alzheon, a biotech company based in Massachusetts, is developing a small molecule treatment (ALZ-801) for people who carry the E4 allele, focusing initially on APOE4 homozygotes. “These patients decline very rapidly once they start showing symptoms, so it’s a very fragile population that we’re trying to help out,” explained Alzheon chief of staff, Adem Albayrak.
ALZ-801 is a prodrug of a previously tested compound known as tramiprosate or homotaurine, which originally comes from seaweed. Tramiprosate reached Phase III trials but did not show enough efficacy to be approved. However, it did show beneficial effects in APOE4 carriers, prompting the development of ALZ-801. The potential therapy is currently being tested in a Phase III trial, which is due for a read-out this year.
“The data we saw in the Phase II study gave us confidence to start building out our commercial capabilities. We’re starting to focus on the regulatory submission, so when the data reads out, we can quickly and efficiently get to the FDA and file for potential approval,” said Albayrak. “We’re trying to prepare the company so we can make it available for patients as quickly as possible if it reads out the way that we’re hoping.”
Alzheon is not the only company focusing on APOE genetics. Lexeo Therapeutics has a focus on gene therapy development for cardiac diseases and Alzheimer’s disease. The New York biotech is developing three separate gene therapies to target Alzheimer’s, the first of which (LX1001) carries the allele for APOE2 and has anti-Alzheimer’s disease properties that can help fight the disease.

“If you’re an E2/E4 heterozygote, the existence of E2 removes E4 risk, and so you go back to normal,” explained Lexeo CEO, Nolan Townsend. “This is the thinking behind the gene therapy program. We’re actually using APOE2 as a therapeutic, which we’re delivering to the central nervous system of E4 homozygotes, seeking to alter their central nervous system to become closer to the E2/E4 heterozygote profile.”
LX1001 is currently in Phase I/II trials and the results of these should be read out by the end of the year. The company is also developing a similar gene therapy (LX1021) containing APOE2 with an additional mutation thought to be protective against the disease and a more complex gene therapy (LX1020) to provide protective APOE2 while simultaneously suppressing APOE4, but both these programs are at very early stages.
Townsend and colleagues believe that correcting the genetics of the disease may have a beneficial effect on many disease outcomes, instead of correcting just one part of the abnormal physiology seen in Alzheimer’s patients.
“In the view of many experts, the pathogenesis of Alzheimer’s is multivariate. Tau, phospho-tau, amyloid beta, inflammation, blood brain barrier abnormalities, there are a number of different pathologies likely involved in this disease,” he explained.
“Focusing on a single pathogenic mechanism may not correct the totality of this very complex disease, so in our view, the way to do that is to go upstream and treat the genetics of the disease, which we expect to have a downstream impact on multiple different pathogenic mechanisms.”
Voyager Therapeutics, based in Massachusetts, is also developing gene therapies to target Alzheimer’s. It has developed a platform called TRACER™ (Tropism Redirection of AAV by Cell-type-specific Expression of RNA) to refine the choice of gene therapy capsid to those that can pass through the blood–brain barrier and effectively target the central nervous system.
Unlike Lexeo, the company is not focusing on APOE genetics, but instead has a tau silencing and a vectorized anti-amyloid beta gene therapy in preclinical development, as well as an anti-tau antibody (VY-TAU01) that will go into clinical trials this year.
Voyager CSO Todd Carter, PhD, emphasized the difficulty of delivery for therapies targeting the brain. “In intrathecal administration, there’s a gradient that forms and you can’t get to some of the deeper structures in the brain… we can dose intravenously and by doing so we can leverage the vascular system… The challenge is the blood brain barrier, but because we’re able to get across it, we should be able to get quite broad delivery through parts of the brain that are very difficult to target.”
Embracing new approaches
The lecanemab approval last year marked what many believe is just the beginning of a new era of novel and more effective Alzheimer’s therapies. Some of the treatments in development, such as the variety of monoclonal antibodies progressing through clinical trials, have been worked on by many researchers for a long time and are following broadly similar methodologies.
However, others are earlier in their development or are following innovative or unique approaches. It is clear that Alzheimer’s is a heterogenous disease that is likely to benefit from a precision medicine approach of designing a variety of therapeutics that will suit different patient groups and could even be used in combination with other therapies.

CEO of New York biotech Cognition Therapeutics
Lisa Ricciardi is CEO of New York biotech Cognition Therapeutics, which, like Acumen, is targeting amyloid beta oligomers, but not using an antibody therapy. Instead, the company is using an orally delivered small molecule to stop amyloid beta oligomers from binding to synapses.
“I am quite excited about the fact that there are so many different approaches,” she commented. “In oncology in the 1960s it was straight chemotherapy and that was brutal. Eventually you added radiotherapy, then came immunotherapy and the whole cocktail approach. I’m very much simplifying oncology, but I do believe we’ll see the same thing in Alzheimer’s disease.”
Ricciardi and colleagues believe that CT1812, Cognition’s candidate drug, has the potential to work well as a combination therapy. For example, with antibodies that act to remove plaque. It is currently being tested at Phase II in mild-to-moderate Alzheimer’s disease patients and results are expected later in the year.

Others, such as AC Immune, are taking a vaccine or immunotherapy approach to solving the problem. Instead of treating people with monoclonal antibody therapies they want to induce the body to produce its own antibodies against the proteins that lead to Alzheimer’s disease.
The company has an anti-amyloid beta vaccine (ACI-24) for generating antibodies against the misfolded amyloid protein in Phase II trials, as well as an anti-phospho-tau vaccine at a similar stage of development that the company has produced in collaboration with Janssen.

Pfeifer and colleagues want to make full use of recent improvements in diagnostics and early Alzheimer’s biomarkers to ensure their vaccines get to those that need them at the right time for disease prevention or early remission, but acknowledge that work is needed to prepare doctors and healthcare systems for this approach.
“We are already reaching out to governments, and we are really active on the community level, because the cost of this disease is becoming more and more of a burden. If you could invest in prevention, it would be a lower investment in the long term,” explained Pfeifer. “But the infrastructure has to be started now. It wouldn’t help us a lot if we develop active immunotherapy and the infrastructure does not exist.”
Vandria is taking a completely different approach to treating Alzheimer’s disease. It is known that one feature of Alzheimer’s disease and other age-related neurodegeneration is an accumulation of damaged mitochondria in the brain.

“There’s a highly selective process where the body has to identify damaged mitochondria, digest them and replace them with healthy mitochondria—a process called mitophagy, which seems to be impaired as we age particularly in certain disease populations,” explained Dugi.
“What we’re trying to do with very selective and potent compounds is to induce this natural process of mitophagy to tackle various diseases, including Alzheimer’s disease.”
The company is still at an early stage of drug development, but it has already seen some promising early results in animal models.
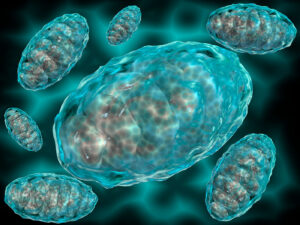
“We have shown an improvement in cognitive function in mice after one hour of treatment,” noted Dugi, “in addition to that, we have seen disease modifying properties in longer term models of Alzheimer’s disease including reduced brain inflammation and reduced aggregation of amyloid beta protein, as well as improved mitochondrial function.”
Predicting the future
The first steps on the road to better treatments for Alzheimer’s disease and other dementias have undoubtedly been taken, but what is next for the field? From a precision medicine perspective, it appears to be following in the footsteps of oncology.
Big advances in the number and type of biomarkers that can be used to predict both disease onset and progression mean it will be easier to design clinical trials and predict who will benefit most from new therapies. This will also help prevention efforts such as those being developed by AC Immune.
“The advent of these biomarkers and our ability to move quickly into the clinic and determine whether these drugs are working is really important to the industry, it allows us to take more shots on goal,” said Carter.
Kinney agreed and noted that “a potential concept of having a blood marker for amyloid that one could continue to look at, like you’d follow your cholesterol levels in the context of cardiovascular disease, is very exciting to think about. Particularly, because what we’re talking about is slowing the progression of this disease.”
In February, an NEJM paper showed that biomarkers for Alzheimer’s can be seen twenty years in advance of disease onset. “If we can identify patients, maybe not twenty years, but five or ten years before overt dementia and can intervene then we will have a better chance of having an impact,” emphasized Dugi.
With so many potential therapeutic candidates in later stage development, and renewed interest and investment in the field after the approval of lecanemab, it seems likely that we will see more therapies being approved in the near future.
However, it is not enough to just develop new therapies. The right infrastructure needs to be in place for widespread adoption to take place and physicians and other healthcare professionals need to be aware of the options that are available to them for treating patients.
“The current late stage and approved therapies require substantial infrastructure that just isn’t out there. For example, MRI monitoring for safety and bi-weekly or monthly infusions. It’s a tremendous burden on patients and on caregivers,” said Albayrak, who advocates for the development of effective oral therapies to help minimize this problem.
Preparation is particularly important if prevention approaches become more common, as there will need to be some way of ensuring early identification of those at risk to ensure that appropriate prevention measures or therapies are given at the right time.
FDA approaches to the approval of therapies still in development will also be key, because a need for large cognitive decline studies may rule out many smaller companies due to the high costs involved.
“My hope is we see the type of flexibility that encourages investment, and that investment will yield more therapeutic options for Alzheimer’s patients,” said Townsend.
“It’s an exciting topic. I think there’s a $40 billion disease area that’s we’re watching emerge here, and tracking how this goes and what impact we see for patients will be an important thing to watch.”
Read More:
- Lecanemab in Early Alzheimer’s Disease—NEJM, Jan 2023
- Roche’s Genentech returns Alzheimer’s assets to AC Immune, cutting 18-year tie to the biotech—Fierce Biotech, Jan 2024
- FDA Converts Novel Alzheimer’s Disease Treatment to Traditional Approval—FDA website, Jul 2023
- FDA’s Decision to Approve New Treatment for Alzheimer’s Disease—FDA website, Jul 2021
- Aduhelm Phase 3 Data: ARIA Is Common, Sometimes Serious—Alzforum website, Dec 2021
- Biogen Will Refocus Its Alzheimer’s Pipeline and Stop Selling Aduhelm—Inside Precision Medicine, Jan 2024
- Lilly’s Donanemab Significantly Slowed Cognitive and Functional Decline in Phase 3 Study of Early Alzheimer’s Disease—Eli Lilly website, May 2023
- Donanemab in Early Symptomatic Alzheimer Disease The TRAILBLAZER-ALZ 2 Randomized Clinical Trial—JAMA, July 17, 2023
- Acumen’s stock surges as early Alzheimer’s data suggest next-gen Leqembi rival is active—Fierce Biotech, July 2023
- Apolipoprotein E and Alzheimer disease: risk, mechanisms, and therapy—Nature Reviews Neurology, Feb 2013
- ApoE in Alzheimer’s disease: pathophysiology and therapeutic strategies—Molecular Neurodegeneration, Nov 2022
- Mitophagy inhibits amyloid-β and tau pathology and reverses cognitive deficits in models of Alzheimer’s disease—Nature Neuroscience, Mar 2019
- Biomarker Changes during 20 Years Preceding Alzheimer’s Disease—NEJM, Feb 2024
Helen Albert is senior editor at Inside Precision Medicine and a freelance science journalist. Prior to going freelance, she was editor-in-chief at Labiotech, an English-language, digital publication based in Berlin focusing on the European biotech industry. Before moving to Germany, she worked at a range of different science and health-focused publications in London. She was editor of The Biochemist magazine and blog, but also worked as a senior reporter at Springer Nature’s medwireNews for a number of years, as well as freelancing for various international publications. She has written for New Scientist, Chemistry World, Biodesigned, The BMJ, Forbes, Science Business, Cosmos magazine, and GEN. Helen has academic degrees in genetics and anthropology, and also spent some time early in her career working at the Sanger Institute in Cambridge before deciding to move into journalism.













