Research led by scientists at the Wellcome Sanger Institute in the UK shows that the production of blood cells changes dramatically after the age of 70 years likely due to a slow build up in mutations over time.
The buildup of mutations in normal, non-reproductive somatic cells over time is believed to be a contributing factor to the aging process, but the specifics of how these gradual mutations impact organ health is still unclear.
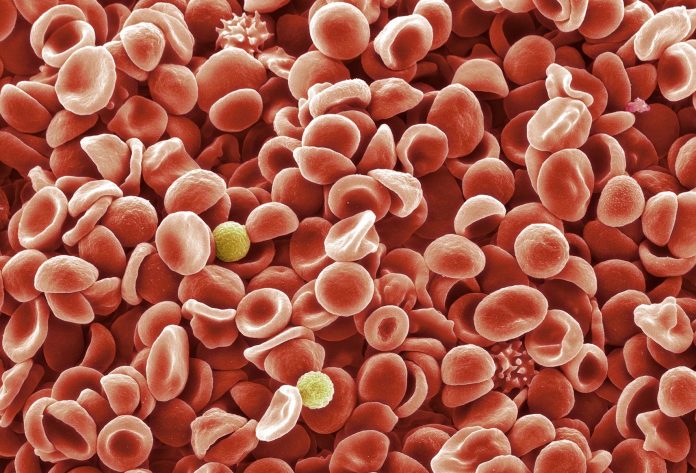
We produce over 2 million blood cells per second, which originate from a group of hematopoietic stem cells (HSCs). Over time these HSCs accumulate small mutations, some of which make the cell more likely to survive and proliferate than others (driver mutations) whereas others have little effect (passenger mutations).
To investigate links between aging and blood cell changes over time, the research team analyzed the production of blood cells from bone marrow in 10 individuals ranging in age from newborn to elderly. The study describing the work was published in Nature, as well as an accompanying study exploring how different driver mutations impact blood cell growth rates.
Overall, the genomes of 3579 blood cells were sequenced and all the somatic mutations were identified. The scientists compared the cells and sequences between the individuals and assessed the impact of age and time on the mutations.
There was a striking difference between the production of blood cells in individuals under the age of 65 and those over 70 years. In those in the younger group, between 20,000-200,000 stem cells contributed equally to the production of new blood cells. Whereas in the older group, blood cell production varied a lot. As few as 10-20 expanded stem cell clones produced as much as half of all the blood cells.
The team think this reduction in diversity is due to the action of selfish ‘driver mutations’ that can result in dramatically reduced cell diversity over time and could be the reason older people are more prone to illnesses and infections. Because the type of driver mutations and resulting cell populations varies from person to person, this could explain some of the variation in health issues seen in older people.
“Factors such as chronic inflammation, smoking, infection and chemotherapy cause earlier growth of clones with cancer-driving mutations. We predict that these factors also bring forward the decline in blood stem cell diversity associated with ageing,” says Elisa Laurenti, Assistant Professor and Wellcome Royal Society Sir Henry Dale Fellow at the Wellcome-MRC Cambridge Stem Cell Institute at the University of Cambridge, and joint senior researcher on this study.
“It is possible that there are factors that might slow this process down, too. We now have the exciting task of figuring out how these newly discovered mutations affect blood function in the elderly, so we can learn how to minimize disease risk and promote healthy ageing.”










