Researchers have described mechanisms involved in focal amplification (FA) of BRAF and other genes in the MAPK signaling pathway, which is a driver of many cancer types. These findings could help further understanding of drug resistance to particular drugs for cancers, including melanoma.
“This study was designed to provide details about the structure, dynamics and vulnerabilities of MAPK-related focal amplifications as they relate to drug resistance in melanoma,” said Kai Song, a graduate student and the article’s first author. “A complete knowledge of these structures and interactions is central to our understanding of tumor evolution and plasticity and to the development of therapeutic approaches that overcome resistance.”
Their article was published online Dec. 20 in Cancer. The senior author was Thomas Graeber, Ph.D., a researcher with the UCLA Jonsson Comprehensive Cancer Center and director of the UCLA Metabolomics Center.
The researchers developed a melanoma model of drug resistance, enabling them to map intrachromosomal and extrachromosomal changes that lead to resistance in cancer cells. The model also allowed them to observe resistance-related responses when they manipulated drug doses.
BRAF mutations, relatively common in thyroid cancer and melanoma, have been targeted using drugs such as vemurafenib and dabrafenib and other MAPK pathway inhibitors. Resistance often occurs, however, through reactivation of this pathway, activation of a different pathway, or both.
One mechanism of MAPK pathway reactivation often seen in melanoma is the acquisition of BRAF amplifications.
The researchers treated a human melanoma cell line with kinase inhibitors that target the MAPK signaling pathway to develop a model of drug resistance. Initially, high BRAF gene amplification was seen in the extrachromosomal DNA form, but over the course of months in culture at a stable drug dose, the mechanism switched to the intrachromosomal HSR form.
According to the authors, the observance of a mode switch in melanoma adds to several related reports in the literature of similar events in focally amplified oncogenes of different cancer types, including leukemia and neuroblastoma.
The study found that each form of DNA offered different ‘fitness’ advantages to tumor cells, such as in response to changing therapeutic conditions. For example, when cells are exposed to constant, steady drug dose treatment, intrachromosomal HSRs appear to be “more fit” than their extrachromosomal counterparts to promote cancer growth – supporting a fitness-driven evolution from DMs to HSRs in these conditions. However, a non-steady or oscillating drug dose challenge creates an advantage for not having the amplicon copy number tied to chromosomes, and thus DM-harboring cells are retained.
The findings were bolstered by reports in the literature and clinical studies from a team led by collaborator Dr. Roger Lo, a member of the UCLA Jonsson Comprehensive Cancer Center. They found evidence for the plasticity of focal amplifications of MAPK genes in patient tumors and in patient-derived xenograft-model tumors that have become resistant to MAPK inhibitor treatments.
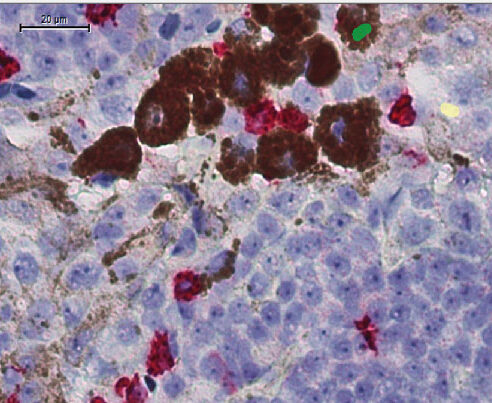
Among other significant results, the research team documented that although melanoma cells may become resistant to signaling pathway-inhibiting drugs, treatment with the drugs appears to make them vulnerable to a different agents. With MAPK inhibition, melanoma cells shift their major energy generation program from glycolysis, or glucose metabolism, to mitochondrial pathways in which respiration and energy production occur within the cells. This leads to elevated production of reactive oxidative stress in the treated cells.
“An important value of this model system is that it is allowing us to hunt for new vulnerabilities of cancer cells that use these focal amplification-based methods of resistance. Therapeutically targeting these vulnerabilities is our end goal,” Graeber said.













