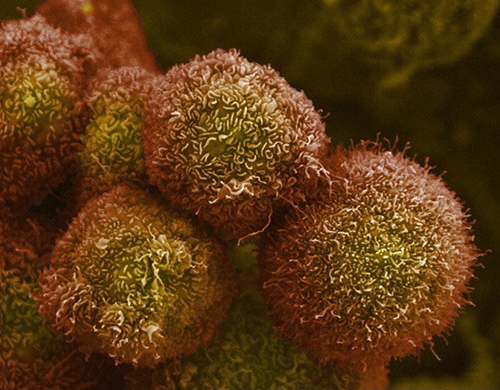
The aggressive nature and treatment resistance of pancreatic cancer stems from its microenvironment that overpowers immune activity (immunosuppression) and surrounds tumors with a protective mesh of dense fibrotic tissue (desmoplasia).
Scientists led by Dafna Bar-Sagi, PhD, a professor of biochemistry and molecular pharmacology at NYU Langone Health, have discovered a regulatory mechanism through which certain immune cells (macrophages) associated with pancreatic tumors engulf and break down collagen in the extracellular matrix to trigger desmoplasia. Reprogramming this cancer-promoting mechanism could alter the composition of the tumor microenvironment and develop new treatment options for this devastating malignancy.
The study was published on April 4, 2022, in an article in the Proceedings of the National Academy of Sciences titled, “Metabolic reprogramming of tumor-associated macrophages by collagen turnover promotes fibrosis in pancreatic cancer.”
“Our group has a long-standing interest in understanding ‘cellular conversations’ between cancer cells and other cell types in the microenvironment and how they influence tumor development,” said Bar-Sagi. “This study was inspired by our discovery that the scavenging of extracellular proteins and their subsequent degradation to amino acids can profoundly affect cellular metabolism.”
Bar-Sagi added, “While originally described in the context of albumin scavenging by tumor cells, the present study determines whether the link between extracellular protein scavenging and cell metabolism can be more broadly applicable to cellular components within the tumor ecosystem, in this particular case, macrophages.”
Structural proteins such as collagen fibers that form a dense supportive net around organs and damaged tissue, are continuously replaced to maintain tensile strength and heal wounds. Earlier studies have shown tumor-associated macrophages play a prominent role in remodeling of regions around tumors via collagen production and degradation. A protein called mannose receptor 1 (MRC1) enables macrophages to engulf and degrade collagen through a process called endocytosis.
“Our results revealed how pancreatic tumors program macrophages to contribute to the construction of fibrotic barriers,” said Madeleine LaRue, PhD, who is the first study author of the study. “This molecular framework could be harnessed to counter pro-cancer changes in structural tissues surrounding tumors.”
The current study found that increased collagen degradation in tumor-associated macrophages increases the amino acid arginine that the enzyme nitric oxide synthase (iNOS) uses as a substrate to produce reactive nitrogen species (RNS), which in turn induces supportive stellate cells (a type of resident stromal cells) to build collagen-based meshes around tumors.
RNS is an umbrella term for a diverse family of highly reactive, unstable, messenger molecules produced by different cell types and are challenging to measure accurately.
“We used a new, highly sensitive live imaging, fluorescence microscopy-based technique developed by Chen et al, 2021, at NYU Chemistry department, to measure the production of RNS at a single cell level in real time. Using this technology, we acquired high-precision measurements of RNS levels in macrophages and demonstrate how different experimental conditions affected RNS production,” said Bar-Sagi.
The researchers conducted experiments that showed cultured macrophages converted into cancer-tolerant states (M2), break down far more collagen than macrophages programed to engulf cancer cells (M1). In a series of tests, the researchers show M2 macrophages have higher levels of enzymes that generate RNS, such as iNOS.
“Our experiments revealed, feeding macrophages with fragments of collagen proteins directly increases their RNS production. These findings provide a biological explanation for how macrophages alter their behavior in response to collagen consumption and the consequences of these changes for other cells in the tumor microenvironment,” said Bar-Sagi.
The researchers then implanted normal stellate cells or stellate cells grown in media with a high level of collagen into the flanks of test animals along with pancreatic cancer cells. They found this doubled the density of collagen fibers in tumors derived from cancer cells co-implanted with stellate cells grown in high collagen.
Bar-Sagi said, “Macrophage phenotype is a critical determinant in tumor development and responses to immune modulatory targeting strategies. The identification of a new mechanism by which macrophage phenotype can be regulated advances our understanding of how the pancreatic tumor immune milieu is shaped and can lead to the identification of immune vulnerability that can be exploited therapeutically to treat a disease with the most dire outcomes.”
The study is the first to show that macrophages near pancreatic cancer cells, not only take in and break down more collagen but are also changed by their scavenging role, such that their metabolism is rewired to promote the buildup of fibrotic tissue.
“Our team uncovered a mechanism that connects collagen turnover to the building of a treatment-resistant environment around pancreatic tumors,” said Bar-Sagi. “As this dense environment is a major reason why pancreatic cancer is so deadly, a better understanding of links between protein scavenging and the building of protective barriers will be needed to improve the treatment of this devastating malignancy.”
In future experiments Bar-Sagi’s team plans to probe into how different RNS molecules produced by macrophages that have ingested collagen influence the behavior of tumor cells and cells in their environment.













