Researchers from the Garvan Institute of Medical Research have released research findings detailing how collagen type XII plays a role the regulation and organization of the cancer tumor matrix and also triggers breast cancer cells from the tumor to spread around the body.
A potential application of this new finding, published in the journal Nature Communications, is for the development of tools or diagnostics that could screen for collagen XII to help identify cancer subtypes with high rates of metastasis—such as triple-negative breast cancer(TNBC)—or as a potential new target for future breast cancer treatments.
The tumor microenvironment is the ecosystem that surrounds cancer tumors which affects how a tumor grows. The tumor matrix is one element of the tumor microenvironment. Collagen is known to play an important role within tumor microenvironment, but its exact role has remained elusive.
“There’s still a lot we don’t know about the role of the extracellular matrix in cancer metastasis,” said senior author Thomas Cox, an associate professor at the Garvan Institute. “Our study shows that collagen XII plays an important role in breast cancer progression and metastasis. Imagine cancer cells as seeds, and the tumor microenvironment as the soil. By studying the soil— the extracellular matrix—we can begin to understand what makes some tumors more aggressive than others, and by extension, begin to develop new ways to treat cancer.”
Uncovering collagen’s role in breast cancer metastasis
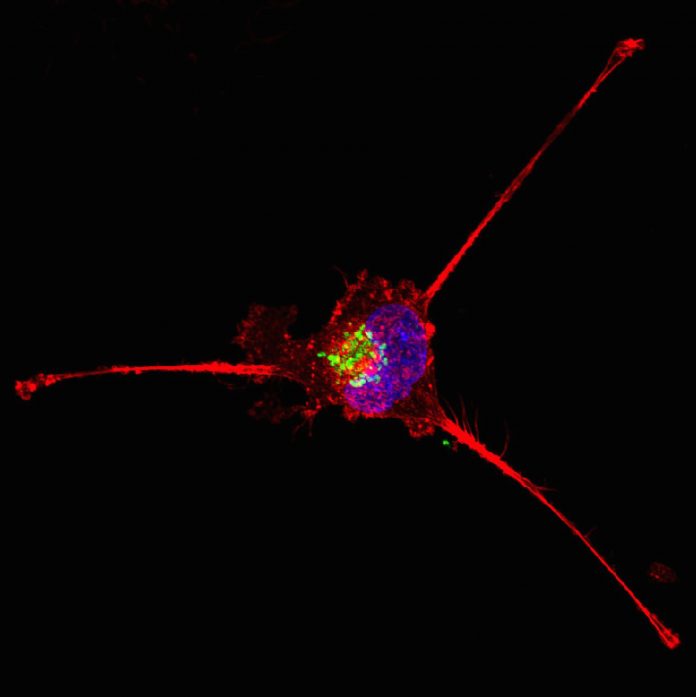
The study by the Garvan researchers was aimed at better understanding the role of the 300 to 400 molecules typically present in the extracellular matrix, a meshwork that provides support to all tissues in the body. The investigators looked to better understand how the tumor matrix changes over time and soon focused on collagen XII, one of 28 collagen types found in the body. Collagen XII helps to organize other collagens and plays an important role in the 3D structure of the extracellular matrix.
Using an array of tumor tissue types from early preclinical mouse models through to late-stage cancer, the Garvan team was able to demonstrate how the molecular makeup of the extracellular matrix changed over the development of tumors and catalogued these findings. They found that as the tumors developed, among the changes of many other matrix molecules, the level of collagen XII was also increased.
To determine the clinical relevance of collagen XII in breast cancer patients, collagen XII expression was analyzed in RNAseq data from the Cancer Genome Atlas (TCGA) breast cancer cohort, which confirmed significant upregulation of collagen XII across all primary breast tumor types, including TNBC, relative to non-tumor tissue.
“Multivariate analysis of collagen XII expression together with corrections for the clinical covariates age, stage, receptor status and the presence of cancer cell positive lymph nodes revealed that collagen XII expression was the strongest predictor for progression-free survival in early stage (Stages I and II) breast cancer compared to these clinical covariates,” the researcher wrote. “However, collagen XII expression was not a significant predictor of overall or progression-free survival when tumours across all stages (I–IV) were examined together, suggesting that collagen XII expression is more strongly associated with early-stage progression.”
The study’s first author, Michael Papanicolaou of the Garvan Institute noted: “Collagen XII seems to be altering the properties of the tumor and makes it more aggressive. It changes how collagens are organized to support cancer cells escaping from the tumor and moving to other sites like the lungs.”
Future studies to the role of collagen XII will seeks to include more humor tumor samples, while also exploring potential therapeutic pathways.
“In recent years, there has been a marked increase in interest in the role of the matrix in defining the properties of the tumor microenvironment, and our findings support the emerging hypothesis that future therapeutic approaches to ‘normalize’ or re-engineer the tumor stroma may offer the potential for significant translational impact in improving patient survival,” the authors wrote.













