Researchers at the Netherlands Institute for Neuroscience and the VIB-KU Leuven Center for Brain and Disease Research have discovered that a tiny molecule called microRNA-132 may play a significant role in the pathology of Alzheimer’s disease.
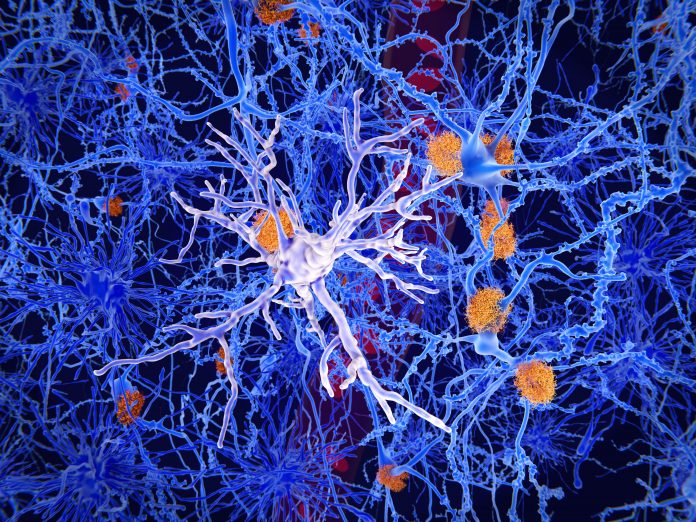
Alzheimer’s disease is typically characterized by the buildup of protein aggregates called amyloid beta plaques in the brain, causing nerve cells to deteriorate and leading to cognitive decline. However, there are several other molecules rumored to be involved in the onset of the condition—one of them being a type of non-coding RNA molecule called microRNA.
Despite not coding for any proteins, microRNA molecules can have a significant effect on cells by binding to RNA molecules and changing the way genes and proteins are expressed. Previous studies have shown that Alzheimer’s patients often show a significant decrease in a type of microRNA known as microRNA-132—associated with an increase in neuroinflammation.
Reporting in iScience, researchers have now investigated the effects of the molecule in different cell types using a technique called single-cell RNA sequencing, allowing them to observe the changes caused by microRNA-132 in specific genes.
“We know that microRNA-132 performs various functions in neurons, but surprisingly, we found that this microRNA also plays a role in microglia, the immune cells of the brain. This is interesting in the case of Alzheimer’s because we believe that neuroinflammation plays a significant role,” said Amber Penning, PhD student at the Netherlands Institute for Neuroscience, and co-author of the study in a press statement.
According to the scientists, increasing levels of the molecule in microglia of mouse and human origin proved beneficial for the cells—shifting them from a disease-associated to a more balanced state. These findings suggest that microRNA-132 plays a role in the process of neuroinflammation that leads to Alzheimer’s disease and could be used as a potential therapeutic target.
“There are different theories suggesting that this disease-associated state may initially aid in cell clearance during the early stages of the disease but becomes excessive later, leading to the death of healthy cells. We still need to determine how beneficial it is for the cells to become more homeostatic. Therefore, we need to be cautious in drawing conclusions,” Penning explained.
As a next step, the researchers aim to examine whether increasing microRNA-132 levels in mouse models of Alzheimer’s disease will have the same beneficial effect as seen in the mouse and human cell lines in vitro.
“The ultimate goal would be to increase microRNA-132 in Alzheimer’s patients as a therapeutic strategy. Currently, we are using viruses (containing the microRNA) in Alzheimer’s mice that can be injected intravenously, directly into the veins.”
“This makes it easier to eventually translate this strategy to the clinic, as we are utilizing a virus that, in theory, can also be injected into an arm. In addition to Alzheimer’s, there are other neurodegenerative diseases that exhibit a decrease in the same microRNA. Therefore, these results may also be relevant to other disease conditions,” Penning concluded in a press statement.











