Research from the University of Pittsburgh School of Medicine suggests that selective deletion mutations drives evolution of the SARS-CoV-2 virus to avoid being targeted and destroyed by neutralizing antibodies from the immune system.
Mutation rate in coronaviruses is actually lower than other viruses such as the flu and HIV because they produce a polymerase ‘proofreading’ enzyme that normally acts to correct mutations such as substitutions, which change the sequence.
However, as demonstrated by Paul Duprex, Ph.D., director of the Center for Vaccine Research at the University of Pittsburgh, and colleagues, this enzyme is less good at detecting gaps in the sequence caused by deletion mutations.
“You can’t fix what’s not there. Once it’s gone, it’s gone, and if it’s gone in an important part of the virus that the antibody ‘sees,’ then it’s gone for good,” explained Duprex.
The researchers have been assessing genetic variants arising in the virus for a while now. They first noticed the tendency for accumulation of deletions in a very sick patient who was ultimately unable to clear the virus.
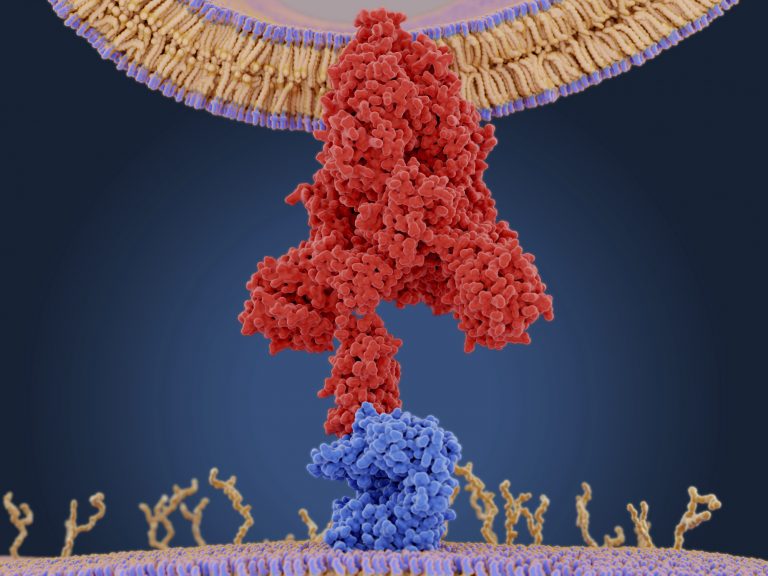
They searched for similar examples in an online database and repository of information on both flu and SARS-CoV-2 called GISAID and found eight patients infected with a strain that initially had no mutations and later acquired deletions in the spike protein – responsible for driving cell infection.
Looking more widely for mutations in the spike protein of the virus, the team found 1108 virus sequences with deletions in the spike protein that were deposited in the GISAID database between December 2019 and October 2020. One notable example of a strain with this kind of deletion is the recently identified B.1.1.7. variant of the virus, identified in the UK at the end of 2020.
As described in the journal Science, around 90% of these mutations were in four specific areas of the gene encoding the spike protein that are known to be involved in antibody response.
Duprex and colleagues hope their findings will be useful for vaccine and drug developers and scientists and clinicians monitoring the spread of the pandemic.
“Going after the virus in multiple different ways is how we beat the shapeshifter,” Duprex said. “Combinations of different antibodies, combinations of nanobodies with antibodies, different types of vaccines. If there’s a crisis, we’ll want to have those backups.”
At the moment none of the variants that have emerged seem to evade the immune system or the currently approved vaccines completely, but there are concerns this might happen in the future. Indeed, the recently identified South African strain does seem to be somewhat resistant to a number of the current vaccines, as demonstrated in recent phase III trials for Novavax and Janssen.
“How far these deletions erode protection is yet to be determined,” commented lead author Kevin McCarthy, Ph.D., assistant professor of molecular biology and molecular genetics at Pitt. “At some point, we’re going to have to start reformulating vaccines, or at least entertain that idea.”













