Patients with glioblastoma (GBM) receiving an immune checkpoint inhibitor who also received dexamethasone at baseline for cerebral edema exhibited significantly worse overall survival, according to a study “Concurrent Dexamethasone Limits the Clinical Benefit of Immune Checkpoint Blockade in Glioblastoma” published recently in Clinical Cancer Research.
“Dexamethasone, a uniquely potent corticosteroid, is frequently administered to patients with brain tumors to decrease tumor-associated edema, but limited data exist describing how dexamethasone affects the immune system systemically and intratumorally in patients with glioblastoma (GBM), particularly in the context of immunotherapy,” write the investigators.
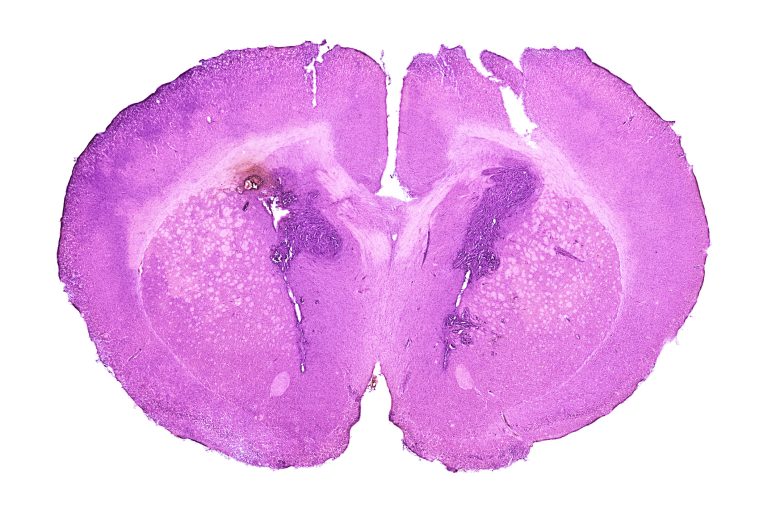
“We evaluated the dose-dependent effects of dexamethasone when administered with programmed cell death 1 (PD-1) blockade and/or radiotherapy in immunocompetent C57BL/6 mice with syngeneic GL261 and CT-2A GBM tumors. Clinically, the effect of dexamethasone on survival was evaluated in 181 patients with isocitrate dehydrogenase (IDH) wild-type GBM treated with PD-(L)1 blockade, with adjustment for relevant prognostic factors.
“Despite the inherent responsiveness of GL261 to immune checkpoint blockade, concurrent dexamethasone administration with anti–PD-1 therapy reduced survival in a dose-dependent manner. Concurrent dexamethasone also abrogated survival following anti–PD-1 therapy with or without radiotherapy in immune-resistant CT-2A models. Dexamethasone decreased T-lymphocyte numbers by increasing apoptosis, in addition to decreasing lymphocyte functional capacity.
“Myeloid and natural killer cell populations were also generally reduced by dexamethasone. Thus, dexamethasone appears to negatively affect both adaptive and innate immune responses. As a clinical correlate, a retrospective analysis of 181 consecutive patients with IDH wild-type GBM treated with PD-(L)1 blockade revealed poorer survival among those on baseline dexamethasone.
“Upon multivariable adjustment with relevant prognostic factors, baseline dexamethasone administration was the strongest predictor of poor survival [reference, no dexamethasone; <2 mg HR, 2.16; 95% confidence interval (CI), 1.30–3.68; P = 0.003 and ≥2 mg HR, 1.97; 95% CI, 1.23–3.16; P = 0.005].”
“Our preclinical and clinical data indicate that concurrent dexamethasone therapy may be detrimental to immunotherapeutic approaches for patients with GBM.”
“Historically, patients with glioblastoma have been empirically treated with dexamethasone, even without symptoms, with many clinicians prescribing steroids for prolonged periods of time, out of a concern that patients may start to develop edema,” said David A. Reardon, MD, clinical director of the Center for Neuro-Oncology at Dana-Farber Cancer Institute in Boston. “Our study was designed to look at that paradigm of clinical practice, particularly in the immunotherapy era, and determine if there could be negative consequences associated with dexamethasone use among patients with glioblastoma treated with immune checkpoint inhibitors.”
In preclinical studies, the team found that steroids had a significant detrimental effect on the efficacy of anti-PD-1 therapy, even in an immunosensitive model, which over-predicts the benefit of immune checkpoint blockade in glioblastoma patients.
The researchers next analyzed overall survival data from 181 patients with glioblastoma treated with either anti-PD-1 or anti-PD-L1 therapy at Dana-Farber Cancer Institute who were diagnosed before April 1, 2019. This patient population was heterogeneous, with patients receiving treatment through a clinical trial or on a compassionate use basis; roughly 76% were treated for recurrence, and roughly 24% were treated for a new diagnosis. Of these 181 patients, around 35% were taking dexamethasone at baseline.
Reardon and colleagues evaluated the potential detrimental effect of dexamethasone using multivariable analysis, where they adjusted for a variety of factors, including disease setting (newly diagnosed versus recurrent), tumor volume at treatment initiation, age, and extent of resection, among the 163 patients that had complete annotated data for relevant prognostic factors. Compared with patients who were not taking dexamethasone at baseline, patients treated with dexamethasone had roughly twice the risk of death. Further, baseline use of dexamethasone was the strongest identified negative risk factor for overall survival.
“Our results suggest that we should try to avoid dexamethasone among patients with glioblastoma who are treated with immunotherapy, and if corticosteroids are clinically required, we should use these drugs judiciously,” Reardon said. “Further, our results highlight that other strategies for the treatment of cerebral edema that do not have such a broad anti-inflammatory effect critically need to be investigated.”
Limitations of the study include the retrospective nature of the clinical analyses. Further, in their preclinical studies, the researchers solely evaluated the effect of dexamethasone on the efficacy of anti-PD-1 treatment.
“Whether the same observations would occur with other immunomodulatory checkpoint targeting agents, or even other immunotherapy treatments—such as vaccines, adoptive cellular therapies, or genetically engineered oncolytic viruses—remains to be evaluated,” noted Reardon.