Multifactorial diseases are notoriously difficult to treat, as their molecular roots are convoluted and enigmatic. Yet in the genomic age, new scientific endeavors are beginning to reveal some interesting connections between seemingly unrelated disorders. For instance, a new study from investigators at the University of California San Diego School of Medicine and the Icahn School of Medicine at Mount Sinai provides insight on the epigenetic landscape for rheumatoid arthritis (RA) and Huntington’s disease. Findings from the new study were published recently in Nature Communications, in an article entitled “Comprehensive Epigenetic Landscape of Rheumatoid Arthritis Fibroblast-Like Synoviocytes.”
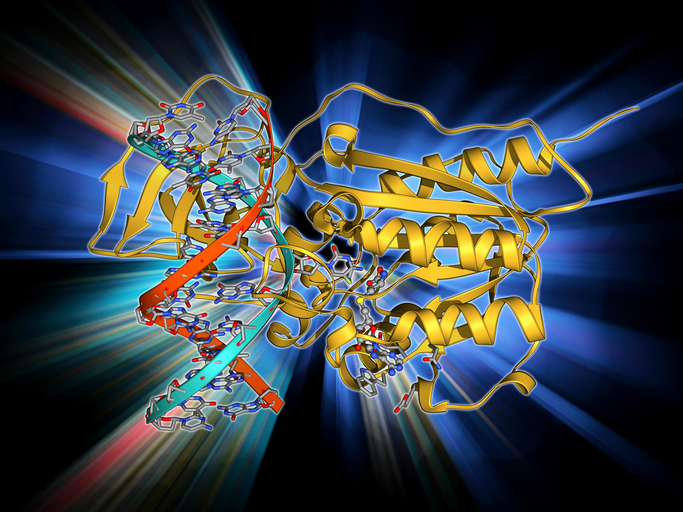
In unveiling RA's epigenome—the proteins and molecules that decorate DNA and help turn genes on and off—scientists made a surprising discovery: an overlap between the causes of RA and Huntington's disease. The researchers noted that the unexpected connection between RA and Huntington's disease opens the possibility of new therapeutic targets and drugs for both conditions.
“We did not expect to find an overlap between rheumatoid arthritis and Huntington's disease, but discovering the unexpected was the reason that we developed this technology,” explained senior study investigator Gary Firestein, M.D., dean and associate vice chancellor of translational medicine at UC San Diego School of Medicine. “Now that we have uncovered this connection, we hope that it opens a door for treatment options for people living with either disease.”
RA is a chronic inflammatory disorder that causes pain and swelling in joints. As an autoimmune disease, it can also affect other organs, including heart and blood vessels. Treatment for RA has improved, but 10% to 20% of patients do not respond to any available medicines.
In the current study, the investigative approach used by the research team involved developing a novel algorithm, or set of computational rules, called EpiSig, which integrated and reduced the number of epigenetic combinations in the genes of patients with RA. The team could then identify new cell signaling pathways.
“Comparing different types of epigenomic data is difficult because it involves a variety of different data subsets that cannot normally be analyzed together, including various methods in which DNA gets modified,” noted co-senior study investigator Wei Wang, Ph.D., professor of chemistry, biochemistry, and cellular and molecular medicine at UC San Diego School of Medicine.
“This methodology can also be used to find connections between other diseases, not just rheumatoid arthritis,” Firestein added. “As genes involved are discovered, researchers can potentially identify new treatment options and even repurpose existing drugs.”
The researchers studied the epigenome in cells from the joints of patients with RA. Patients with osteoarthritis, which is a disease of cartilage degeneration, served as a control group. Both datasets were analyzed through an expansive process that examines chromatin, DNA, and histone modifications. The results produced 12 terabytes of data (12 trillion bytes), which was then analyzed using EpiSig.
“Here we show the first comprehensive epigenomic characterization of RA fibroblast-like synoviocytes (FLS), including histone modifications (H3K27ac, H3K4me1, H3K4me3, H3K36me3, H3K27me3, and H3K9me3), open chromatin, RNA expression and whole-genome DNA methylation,” the authors wrote. “To address complex multidimensional relationship[s] and reveal epigenetic regulation of RA, we perform integrative analyses using a novel unbiased method to identify genomic regions with similar profiles. Epigenomically similar regions exist in RA cells and are associated with active enhancers and promoters and specific transcription factor binding motifs.”
Epigenetics, or “above the genome,” is the study of processes that alter the gene structure without changing the DNA sequence itself. These DNA modifications are essential to human growth and development and change throughout people's lives. Epigenetic changes are influenced by a variety of environmental factors, including stress, activity, and lifestyle choices.
“By revealing the comprehensive epigenetics behind RA, we now have a better understanding of this disease. More importantly, our new approach could not only help patients with RA, but also people with other immune-mediated diseases,” Firestein concluded.











