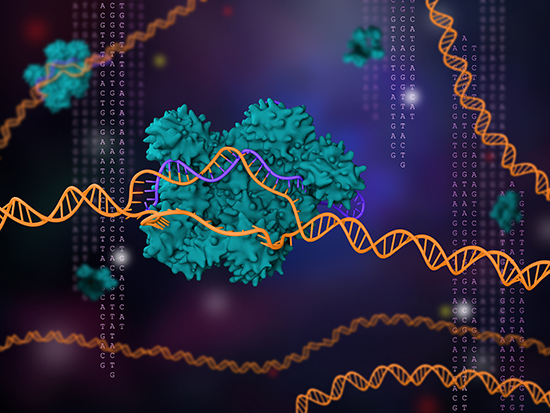
Cedars-Sinai investigators used CRISPR/Cas9 to identify a gene that plays a pivotal role in the innate human immune system. The gene, NLRP11, helps activate the inflammatory response that signals the body’s white blood cells to attack a foreign presence. They determined that NLRP11 is an NLRP3 inflammasome component in human macrophages.
They suggest that being able to influence the expression of the NLRP11 gene may be a key to controlling the inflammatory response and preventing chronic inflammation.
The findings were published this week in Nature Immunology.
“Chronic inflammation is an underlying cause of innumerable human diseases,” said Christian Stehlik, PhD, a co-senior author of the study and director of Pathology Research at Cedars-Sinai. “If you study the molecular mechanisms involved in how inflammation occurs and how it is regulated, you find something that can be applied very broadly.”
When the immune system senses a bacteria, virus, toxin or other foreign presence in the body, it sends white blood cells to surround the unwanted substance and release chemicals to attack it. This response leads to inflammation, which causes redness, pain, warmth and swelling in the affected area as the body heals itself. Sometimes this defensive response lasts longer than it should, resulting in chronic inflammation. Or, the immune system may mistakenly attack healthy cells, leading to autoimmune disease.
“Acute inflammation is necessary and beneficial to eradicate infection and initiate wound healing,” said Andrea Dorfleutner, PhD, co-senior author of the study and associate professor in the departments of Academic Pathology and Biomedical Sciences at Cedars-Sinai. “Chronic, long-term, uncontrolled inflammation, however, is detrimental and can damage the body’s organs and tissues.”
NOD-like receptor (NLR) family pyrin domain containing 3 (NLRP3) is a prominent inflammasome sensor of microbial patterns, internal danger signals, and environmental cues. Excessive or mutation-driven NLRP3 responses cause a wide range of inflammatory diseases, including Cryopyrin-associated periodic syndrome (CAPS), a rare hereditary inflammatory disorder.
NLRP3 inflammasome activation proceeds with first the upregulation of inflammasome components, including NLRP3 and the substrate IL-1β. Next there is a metabolic shift from oxidative phosphorylation to glycolysis and the post-translational modification of NLRP3, ASC and caspase-1.
These investigators used CRISPR/Cas9 to remove genes or introduce gene mutations into macrophages. They observed that when they deleted NLRP11 it prevented the NLRP3 inflammasome from being activated and launching the inflammatory response.
When the researchers restored the NLRP11 gene, the NLRP3 inflammasome resumed sending attack signals, which triggered the typical inflammatory process. The team chose to focus on this gene in particular because it is not expressed in mice, which led them to hypothesize that it was integral to the complex immune system that exists in humans.
“Now that we have a better picture of the mechanisms behind inflammation, we can come up with completely new strategies to target it that have not been possible before,” Dorfleutner said.
The first authors of the study are Anu Gangopadhyay, Savita Devi, PhD, and Shivendra Tenguria, PhD, all investigators in the Stehlik and Dorfleutner Laboratory.











