International research shows that mutations in the gene encoding ubiquilin-2, linked with the serious neurologic condition amyotrophic lateral sclerosis (ALS), can stop the body from discarding misfolded proteins that can build up and destroy nerve cells, and may also cause symptoms of dementia.
The scientists hope that their research can help guide the development of a treatment for ALS, which currently has no cure and is normally fatal.
More than 5,000 people in the USA are diagnosed with ALS, also known as Lou Gehrig’s disease, each year. People with this condition gradually lose the use of their muscles, which can be fatal once the disease begins to seriously impact breathing and swallowing. Around half of those affected also experience dementia-like symptoms.
Mutations in more than 20 genes, as well as some environmental factors, have been linked to ALS onset. It was already known that mutations in the gene encoding ubiquilin-2 — UBQLN2 – were linked with ALS in some people, but the physiological process involved in this was less clear. As described in a paper published in the journal PNAS, researchers have now shown how these mutations can cause disease.
“We mapped out the process by which UBQLN2 gene mutations disrupt an important recycling pathway that cells use to get rid of their trash,” said Mervyn Monteiro, PhD, Professor of Anatomy and Neurobiology, at the University of Maryland School of Medicine, a senior author of the study.
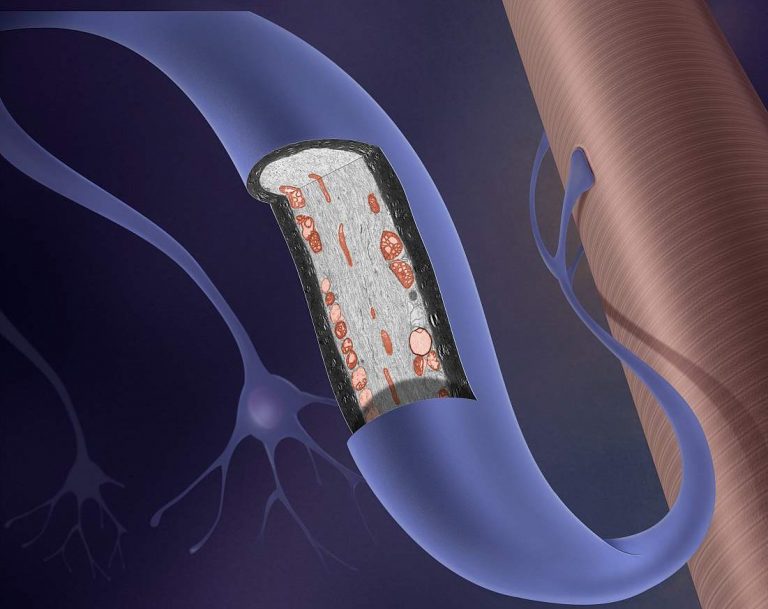
“Without this recycling, misfolded proteins build up in the nerve cell and become toxic, eventually destroying the cell.”
The team studied both human cell lines and mouse models, comparing cells with the UBQLN2 mutation with normal cells. They found that a process called ‘autophagy’, through which the body gets rid of dysfunctional proteins, or parts of the cell or tissues, was not working properly in cells with the mutation. A protein called ATP6v1g1, needed for the cellular breakdown process to regulate acidification, was too low.
Loss of function of the UBQLN2 protein, through one of five disease-causing mutations in the gene, caused a build of cellular ‘rubbish’ that over time could cause symptoms of ALS. Notably, the team found that over expressing the ATP6v1g1 protein in the cell line that had lost UBQLN2 function could start-up the autophagy process again, suggesting a possible treatment method for people with UBQLN2-linked ALS.
The researchers think their findings could have broad implications and may also explain the dementia-like symptoms seen in some patients with ALS.
“Our new findings are exciting because similar acidification defects have been found in Alzheimer’s, Parkinson’s and Down syndrome,” explained Monteiro.
“This suggests that restoration of the defect could have broad implications for not only treating ALS, but possibly other neurodegenerative diseases as well.”












