An international team of researchers has identified a fecal microbiome signature that is specifically associated with pancreatic cancer and has the potential to be used as a cost-effective test for pancreatic cancer screening.
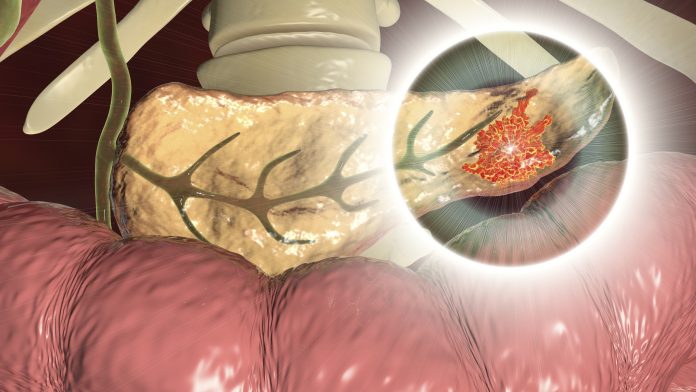
Pancreatic ductal adenocarcinoma (PDAC), the most common form of pancreatic cancer, is a major cause of cancer-related deaths despite relatively low incidence rates because unspecific early symptoms mean it is often diagnosed at a late stage. The 5-year survival rate is less than 10%.
The disease is currently diagnosed using imaging tests, but researchers say there is a need for sensitive, affordable, non-invasive tests that can detect PDAC earlier and thus improve outcomes.
Previous studies have suggested that alterations in the balance of microbial species living in the mouth, gut, and pancreas have been associated with an increased risk for PDAC.
To investigate further, Núria Malats, from the Spanish National Cancer Research Center in Madrid, and Peer Bork, from the European Molecular Biology Laboratory (EMBL) in Heidelberg, Germany, led a collaborative genomic sequencing study to characterize the microbiomes of individuals with PDAC and see if they could be used as an early indicator of disease.
The discovery phase of the study included 57 people with PDAC, 29 individuals with chronic pancreatitis – a known risk factor for PDAC – and 50 healthy controls who provided saliva, stool, and pancreatic issue samples for analysis.
Malats and colleagues found that the gut microbial signatures of individuals with PDAC were significantly different to those of controls or people with chronic pancreatitis.
“These signatures contained some ’usual suspects’ that have previously been associated with other disease,” said Sebastian Schmidt, who is second author on the study and a member of Peer Bork’s laboratory at EMBL. “For example, some bacterial species whose depletion is often associated with intestinal inflammation were also depleted in PDAC patients,”
He added that the team then narrowed down their analysis to microbes that were specific to PDAC. “As a result, our models can identify PDAC patients with good accuracy, but they do not erroneously predict PDAC among other disease groups, including PDAC risk factor groups (chronic pancreatitis patients or type-2 diabetics) and diseases with related symptomatology (such as liver diseases or other cancer types),” Schmidt told Inside Precision Medicine.
Indeed, a panel of 27 microbial species had an accuracy of 84% when used to classify the participants with PDAC in the discovery data set. This increased to 94% when combined with serum levels of carbohydrate antigen 19-9, the only biomarker currently approved for PDAC, despite its limited specificity, the researchers report in Gut.
Among the microbial species included in the panel were Methanobrevibacter smithii, Fusobacterium nucleatum, Alloscardovia omnicolens, Veillonella atypica, and Bacteroides finegoldii, which were all abundant in the stool samples of the PDAC patients along with Faecalibacterium prausnitzii, Bacteroides coprocola, Bifidobacterium bifidum, and Romboutsia timonensis which were depleted.
The accuracy of the panel was validated in a German cohort of 44 patients with PDAC and 32 matched controls and also using publicly available gut genomic data from 5792 individuals with nine different health conditions including other cancers, inflammatory bowel conditions, and type 2 diabetes as well as healthy controls.
Despite the positive findings, both Malats and Schmidt stress that the data are strictly observational.
“Prospective cohort studies are needed to prove that the identified species are present years before the cancer appears and that they predict its appearance. However, at present, there is no cohort study large enough with the sufficient follow-up and, importantly, with stool samples, that allows to rapidly prove that the identified microbiome signature can be translated into screening interventions. These resources need to be built,” said Malats.
Schmidt added that the team identified the same pattern of microbes in patients’ saliva, healthy pancreatic tissue, pancreatic tumors, and gut which he says provides “new angles to study the microbiome’s role in PDAC etiology, but also possible new therapeutic avenues.”
While additional studies take place, the collaborators have applied for a patent to develop a diagnostic kit for PDAC that detects these microbial genomes in stool samples.
“The kit, if commercialized, would be of use in screening interventions to diagnose pancreatic cancer at very early stages,” said Malats.
Schmidt believes the fact that the test would be rapid, non-invasive, relatively inexpensive test is a “major advantage.”
“Such a screen could initially target risk groups, e.g., above a certain age or with a family history of PDAC,” he remarked, adding that “with further development and in combination with other biomarkers, our approach might be developed into an actionable diagnosis method in the future.”













