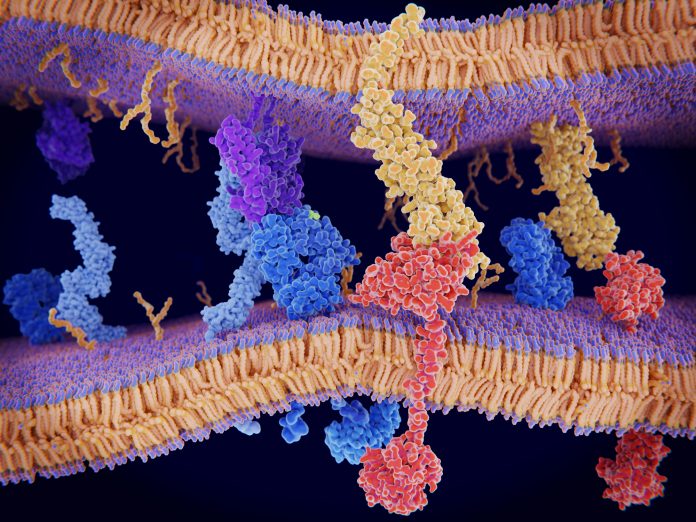
New light has been shed on programmed death receptor ligand-1 (PD-L1) and how its intracellular signaling affects immune suppression and cancer progression. A team from the University of Colorado School of Medicine studied the interactome, or group of proteins with which the intracellular domain of PD-L1 interacts. They found that upon PD-1 binding, the PD-L1 extracellular and intracellular domains exert a synchronized effect to promote immune evasion by inhibiting T cell function while simultaneously enhancing cancer cell invasive properties.
This is critical work, as PD-1 and PD-L1 inhibitors can be extremely effective in a range of cancers, but only in a subset of patients, and often they stop working. Results of this research were published June 30 in the Journal of the National Cancer Institute.
“We found that PD-L1 interacts with a group of proteins when its extracellular domain is free (unbound) that maintain a baseline growth signal, but that when PD-L1 binds to PD-1 (leading to T cell anergy extracellularly) the intracellular domain then increases the number and scope of its interactions, ultimately sending more pro-growth and pro-invasion signals inside the cancer cell,” senior author Antonio Jimeno, MD, PhD, told Inside Precision Medicine. Jimeno is director of the Head and Neck Cancer Program at University of Colorado School of Medicine.
There are several PD-L1 inhibitors approved for multiple indications. The world market for these drugs is estimated to be worth almost $40B. But until recently, intrinsic PD-L1 signaling in cancer has been poorly understood.
“We’re offering a more in-depth view of the cancer and immune cell interaction. This is important because by better understanding immunotherapy-driven signaling, we can better treat patients who haven’t had success with immunotherapy. Our findings show we can potentially achieve tumor control and provide patients with more successful cancer treatments,” said Jimeno.
Jimeno’s research is focused on head and neck squamous cell cancer. Currently, PD-L1 treatment is effective for less than 20% of such patients. But Jimeno says the team’s findings can be applicable to other cancers as well, since the interaction of PD-1 and PD-L1 is such a well validated immune target in human cancers.
Jimeno’s and his team found that upon binding to PD-1, PD-L1 triggers signaling that intrinsically alters the cancer cell phenotype, in addition to impacting the immune milieu. PD-L1 does this by direct interaction of its cytoplasmic domain with a group of intracellular proteins (the PD-L1 interactome) that were characterized in detail using a proximity labeling approach in live cells from several patients.
PD-1 and PD-L1 interaction led to increased STAT3 signaling resulting in higher cancer cell clonogenicity, motility, and invasion, as well as resistance to radiation and chemotherapy. The in vitro results were validated using a pharmacological inhibitor of STAT3, the main PD-L1 interactome partner, in humanized mice bearing tumors donated by Coloradans with head and neck cancer.
“That we found that the PD-L1 interactome is so broad and impacts so many signaling pathways in such a consistent way may indicate that PD-L1 can influence many intracellular processes, and not just be a ligand extracellularly,” said Jimeno. “By dissecting these complex interactions we may be able to glean mechanisms explaining why some cancers never respond (primary resistance) or relapse after an initial therapy response (acquired resistance).”
He added that, “The dissection of PD-L1 cancer and immune cell interaction is much more coordinated and has wider and deeper implications than we thought. This is an evolutionary efficient and elegant mechanism for the cancer cell to trigger invasion once immune evasion has been achieved.”













