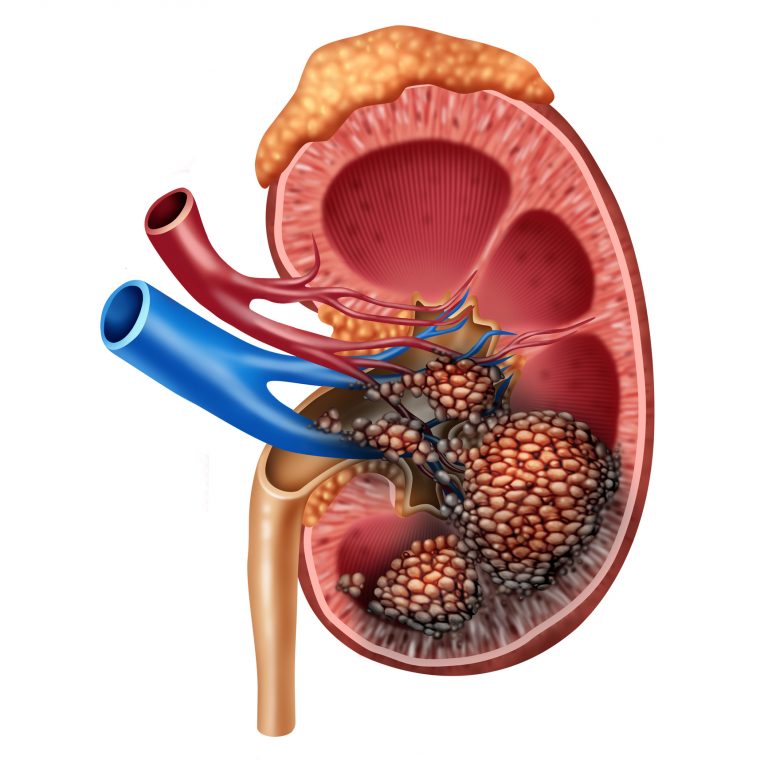
Many patients with clear cell renal carcinoma—the most common type of kidney cancer—eventually experience cancer recurrence and develop incurable metastatic disease. Now, a new study by researchers at Columbia University Vagelos College of Physicians and Surgeons shows promise in predicting which patients are likely to have their cancer recur after surgery.
Their findings are published in the journal Cell, in a paper titled, “Single-Cell Protein Activity Analysis Identifies Recurrence-Associated Renal Tumor Macrophages.”
The researchers demonstrate that the presence of a rare and previously unknown type of immune cell in kidney tumors can predict which patients are likely to have cancer recurrence.
“Our findings suggest that the presence of these cells could be used to identify patients at high risk of disease recurrence after surgery who may be candidates for more aggressive therapy,” explained co-senior author Charles Drake, MD, PhD, adjunct professor of medicine at Columbia University Vagelos College of Physicians and Surgeons and the Herbert Irving Comprehensive Cancer Center.
It’s like looking down at Manhattan and seeing that large numbers of people from all over travel into the city every morning, stated Aleksandar Obradovic, an M.D./Ph.D. student at Columbia University Vagelos College of Physicians and Surgeons and the study’s co-first author. “To understand how these diverse commuters are interacting with Manhattan residents, we need finer details: Who are they; what are they like, where do they go, and what are they doing?”
The researchers first used single-cell RNA sequencing to uncover the finer details of the immune cells that infiltrate kidney cancers. “In many experiments, single-cell RNA sequencing misses up to 90% of gene activity, a phenomenon known as gene dropout,” Obradovic added.
The researchers then addressed gene dropout by developing a prediction algorithm that can infer which genes are active by looking at the expression of other related genes. “Even when a lot of the data are missing due to dropout, we still have enough clues to infer the activity of the upstream regulator gene,” Obradovic said. “It’s like playing ‘Wheel of Fortune’: I can usually guess what’s on the board even when most of the letters are missing.”
The algorithm, meta-VIPER, builds on the VIPER algorithm developed in the laboratory of Andrea Califano, PhD. Califano is the Clyde and Helen Wu professor of chemical and systems biology and director of the JP Sulzberger Columbia Genome Center in the Herbert Irving Comprehensive Cancer Center.
With the addition of metaVIPER, the researchers estimate they can accurately detect the activity of 70% to 80% of all regulatory genes in each cell, eliminating dropout across cells.
These two approaches allowed the researchers to analyze 200,000 tumor cells and normal cells in adjacent tissue taken from eleven patients with clear cell renal carcinoma who underwent surgery in the department of urology at Columbia.
The researchers observed a unique subpopulation of immune cells found only in tumors and associated with eventual relapse of disease after initial treatment. The VIPER analysis uncovered the top genes that control the activity of these immune cells. This “signature” was validated in a second set of patient data obtained through a collaboration with researchers from Vanderbilt University; here the signature strongly predicted relapse in a second set of over 150 patients.
“These data raise the intriguing possibility that these macrophages are not just markers of more risky disease but may actually cause the disease to recur and progress,” Obradovic said, “and that targeting these cells could improve clinical outcomes.”
“Our study demonstrates that the two techniques, when combined, are highly effective at characterizing the cells within a tumor and in surrounding tissues and should have broad applicability, even beyond the study of cancer,” Drake said.













