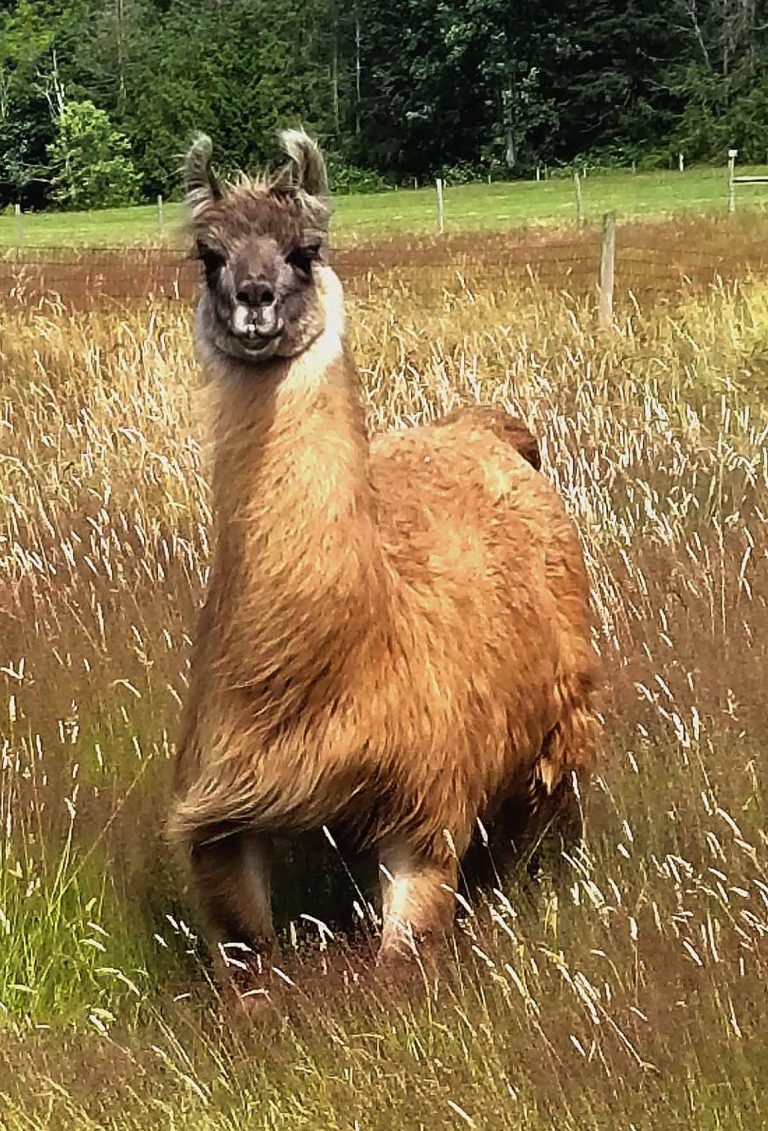
With relatively few therapeutic methods of against COVID-19 currently available, treating patients who develop the disease continues to be a challenge. Now, researchers at the National Institutes of Health (NIH) have isolated a set of promising tiny antibodies called nanobodies that were produced by a llama named Cormac.
A preliminary report of data published in Nature Scientific Reports (“High affinity nanobodies block SARS-CoV-2 spike receptor binding domain interaction with human angiotensin converting enzyme”) shows how one of the nanobodies could both be developed as a therapeutic and as a diagnostic tool to identify COVID-19. The nanobody, dubbed NIH-CoVnb-112, grabs hold of SARS-CoV-2 spike proteins neutralizing its ability to attach to ACE receptors.
The research is the latest to focus on using llama nanobodies against the SARS-C0V-2 spike protein as a method of preventing infections.
Led Thomas J. “T.J.” Esparza, B.S., and David L. Brody, M.D., Ph.D., neuroscientists who work in a brain imaging lab at the NIH’s National Institute of Neurological Disorders and Stroke (NINDS), the pair took a different approach from previous studies to identify nanobodies with therapeutic potential.
“The SARS-CoV-2 spike protein acts like a key. It does this by opening the door to infections when it binds to a protein called the angiotensin converting enzyme 2 (ACE2) receptor, found on the surface of some cells,” said Esparza, the lead author of the study. “We developed a method that would isolate nanobodies that block infections by covering the teeth of the spike protein that bind to and unlock the ACE2 receptor.”
In order to do this, Esparza and Brody immunized the llama Cormac five times over the course of 28 days with a purified version of the SARS-C0V-2 spike protein. They then screened hundreds of nanobodies produced by Carmac, eventually focusing on 13 that could be strong candidates for blocking infections.
The team then screened these 13 contenders against a harmless, engineered psuedovirus in order to use the spike proteins to infect cells with the human ACE2 receptors. Test tube studies showed that the NIH-CoVnb-112 nanobody bound to the ACE2 receptor 2 to 10 times stronger than nanobodies produced by other labs. Other experiments suggested that the NIH nanobody stuck directly to the ACE2 receptor binding portion of the spike protein.
To show that NIH-CoVnb-112 nanobody could prevent infection, the researchers genetically mutated a harmless “pseudovirus” in order to use the spike protein to infect cells that have human ACE2 receptors. The pair observed that relatively low levels of the NIH-CoVnb-112 nanobody prevented the pseudovirus from infecting these cells in petri dishes.
Perhaps most importantly, NIH-CoVnb-112 was as effective at preventing infection when applied with a nebulizer such as those used for treating asthma, providing potentially fast, effective, and inexpensive method for treating patients.
“One of the exciting things about nanobodies is that, unlike most regular antibodies, they can be aerosolized and inhaled to coat the lungs and airways,” said Brody.
While NIH CoVnb-112 shows promise, the researchers note that significant effort will be needed to characterize and develop the nanobody. “We have demonstrated successful neutralization assays involving pseudotyped lentivirus and authentic SARS-CoV-2 isolate neutralization assays are currently underway. Future activities include performing detailed structural and biophysical characterization involving Cryo-EM, X-ray crystallography, in vivo pharmacokinetics and stability assessment, immunogenicity determination, framework humanization, assessing multimerized formats, and further storage and delivery stability assessments,” the researchers wrote.
In addition to therapeutic applications, an inexpensive binding reagent such as NIH-CoVnb-112 nanobody could be used diagnostically. Antibody-based tests could be used to assess for SARS-CoV-2 spike protein in body fluids and the environment. The low cost and temperature stability of nanobodies would be advantageous in some settings, though it is unlikely that antibody-based tests will replace current PCR-based testing for routine clinical use.













