Researchers from the University of Washington and the Fred Hutchinson Cancer Research Center have found that almost half of people considered high risk for lung cancer following computed tomography (CT) screening do not receive follow-up care within the recommended time frame.
“The fact that nearly half of all patients with abnormal findings in our study experienced delays in following up is alarming,” said Alwiya Ahmed, internal medicine resident at the University of Washington School of Medicine, ahead of her presentation at the American Thoracic Society 2022 conference.
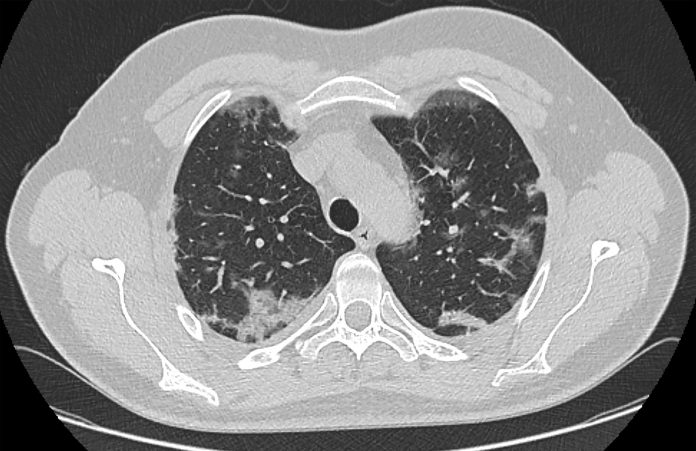
Lung cancer is the leading cause of cancer death and screening is currently recommended by the US Preventive Services Task for adults aged between 50 and 80 years who have a 20 pack–year smoking history and are either current smokers or have quit smoking within the past 15 years.
Ahmed told Inside Precision Medicine that recent studies have looked at why certain populations are not initially screened as recommended under the guidelines, and although these studies have provided important information on specific groups with low screening rates, they do provide information about what happens after screening.
“Our research is aimed at understanding what delays exist in that next step in the process—particularly for those with positive findings that may represent lung cancers. Understanding these delays, and then minimizing them, is crucial in ensuring that disease progression does not unnecessarily occur,” Ahmed said.
Her study included data for 397 patients who had high-risk findings on CT—defined as Lung-RADS 3, 4A, 4B or 4X—after a total of 464 baseline or annual lung screening examinations in a Seattle-based program between 2012 and 2021. Of these, 15% ultimately developed lung cancer.
When the researchers looked at the time from the screening result to follow-up with either a second CT image, other appropriate imaging, specialty consultation, or a procedure, 47% experienced a delay in follow-up.
Specifically, 58% of individuals with a LungRADS3 result, the lowest of the high-risk groups, had a delay of more than 30 days beyond the recommended 6-month interval. In addition, 35% of people with a LungRADS4A finding had a delay of more than 30 days over the recommended 3-month follow-up period, and individuals with a LungRADS4B or 4X result, at the highest risk for lung cancer, had to wait more than 30 days for follow-up. The median times to follow-up were a corresponding 181 days, 68 days and 32 days.
Ahmed and team also investigated whether any patient characteristics were associated with follow-up delays and found that current smokers, who comprised approximately half of the cohort, had significantly higher levels of delay overall than former smokers.
Ahmed suggests that this could be because “current smokers can have a ‘fatalistic’ attitude towards lung cancer and think that if they get it, it is somehow expected and deserved.”
“So, I worry they don’t engage in as much preventive care and follow-up because of this attitude and the stigma associated with ongoing smoking,” she said.
Additionally, men had a higher risk for delay compared to women but there was no significant association with co-morbidities such as cardiovascular disease and diabetes, insurance status, or access to safety net clinics.
The data show that that “interventions are needed at both the provider and patient levels to ensure high-risk patients receive adequate follow-up,” said Ahmed.
She suggests: “At the provider level, education on the importance of follow-up screening and management of abnormal findings may be essential to improve provider comfort at managing these findings and understanding when to refer for further testing. At the patient level, incorporating messaging around the importance of follow-up and adherence to screening during the shared decision-making process would ensure that patients in fact understand the purpose and schedule of these screenings.













