To understand the molecular interplay between the SARS-CoV-2 virus and human tissue, particularly host responses to infection, researchers from the University of California San Diego School of Medicine developed lung and cerebral organoids. When challenged with form of the virus, the organoids’ responses mimicked those found in natural organ tissues perhaps providing researchers a new tool to understanding COVID-19 pathogenesis.
Generated from human induced pluripotent stem cell (iPSC), the team created lung organoids and cerebral organoids to study the reactions of neural progenitor cells (NPCs), neurons, and astrocytes to infection. The team chose to create cerebral tissue organoids to gain insight into why some people with COVID-19 experience cognitive symptoms, like brain fog. Neural cells were studied due to evidence that some people with COVID-19 experience neurological symptoms.
To follow the organoids’ responses to infection, the team developed a pseudovirus — a noninfectious version of SARS-CoV-2 — and labeled it with green fluorescent protein (GFP), to visualize the inner workings of cells. The fluorescent label allowed them to quantify the binding of the virus’ spike protein to ACE2 receptors in human lung and brain organoids, and evaluate the cells’ responses. The team ultimately validated their findings by applying live, infectious SARS-CoV-2 to lung and brain organoids in a Biosafety Level-3 laboratory.
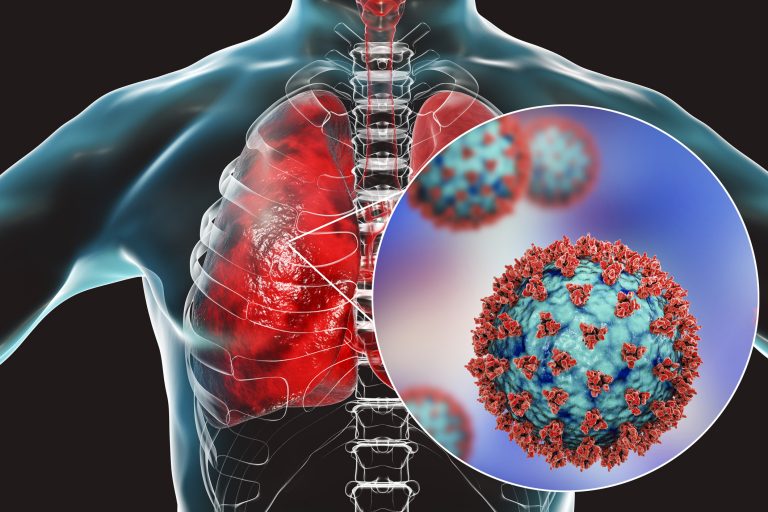
The lung organoids were engineered to contain epithelial cells and alveolar types 1 and 2. They also express ACE2 and TMPRSS2, two molecules the virus uses to first infect a lung cell. When challenged with the virus, the lung organoid responded as expected by allowing the virus to infect the cells. In addition, in response to infection, most of the key genes in innate immunity, cytokine/chemokines, and inflammasome were upregulated in lung organoids.
The team discovered nearly the reverse in other organoids. The cerebral organoids, NPCs, neurons and astrocytes express ten-fold lower levels of ACE2 and TMPRSS2. Infection rates were lower in these cells.
Besides differences in infectivity levels, the lung and brain organoids also differed in their responses to the virus. SARS-CoV-2-infected lung organoids excreted molecules intended to summon help from the immune system — interferons, cytokines and chemokines. Infected brain organoids, on the other hand, increased production of other molecules, such as TLR3, a member of the toll-like receptor family that plays a fundamental role in pathogen recognition and activation of innate immunity.
“We’re finding that SARS-CoV-2 doesn’t infect the entire body in the same way,” said Tariq Rana, PhD, professor and chief of the Division of Genetics in the Department of Pediatrics at UC San Diego School of Medicine and Moores Cancer Center. “In different cell types, the virus triggers the expression of different genes, and we see different outcomes.”
To see if they could block organoid infection by SARS-CoV2, the researchers exposed the cells to several inhibitory compounds. They observed that a spike protein inhibitor called EK1 peptide, and TMPRSS2 inhibitors (camostat and nafamostat) reduced viral entry in both lung and cerebral organoids.
Encouraged by these inhibitory results, the team is now concentrating on using this system to create and test new SARS-CoV-2 inhibitors, particularly in organoid models derived from people of a variety of racial and ethnic backgrounds.













