Biomedical engineering researchers at the Washington University McKelvey School of Engineering, St. Louis have applied a variety of imaging method to diagnose ovarian caaner more accurately. Now, the team from the lab of Quing Zhu, a professor of biomedical engineering, have used machine learning to leverage ultrasound features of ovarian lesions to train a new model that can recognize whether a lesion is benign or cancerous using reconstructed images taken from photoacoustic tomography.
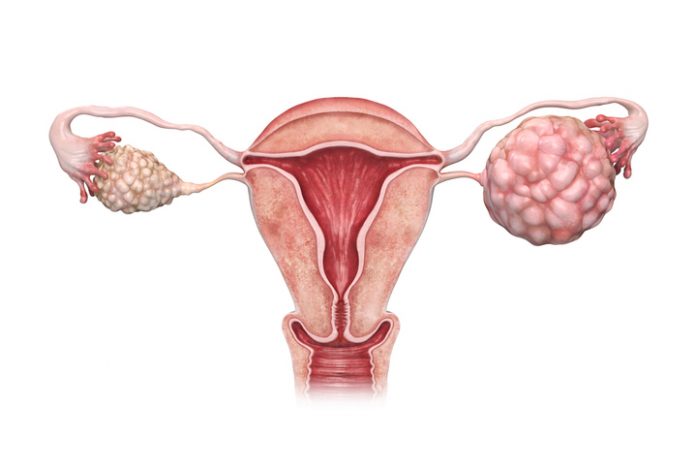
“Compared with benign lesions, malignant lesions often have more numerous solid nodules growing from the cyst wall, more irregular solid components both inside and/or at the lesion periphery, and more blood vessels revealed by Doppler ultrasound,” the researchers wrote. “Although these features are predictive of malignancy…they are not sensitive and specific. Here, we sought to improve overall ovarian cancer diagnosis by using additional functional information obtained from co-registered photoacoustic imaging.”
While ovarian cancer is the deadliest type of cancer for women, only about 20% of cases are found at an early stage, as there are no real screening tests for them and few symptoms to prompt them. Additionally, ovarian lesions are difficult to diagnose accurately — so difficult, in fact that there is no sign of cancer in more than 80% of women who undergo surgery to have lesions removed and tested.
To date, machine learning algorithms have typically employed single modality data, but recent research has shown that multi-modality machine learning is more robust in its performance over unimodality methods. The Washington University study, published in the journal Photoacoustics, is purportedly the first using ultrasound to enhance the machine learning performance of photoacoustic tomography reconstruction for cancer diagnosis.
In a pilot study of 35 patients participated in the study to evaluate the method from February 2017 to November 2018. The patients ranged in age from 33 to 87, and the ovarian lesions’ diameters ranged from 1.8 cm to 11.5 cm. In total these patients had more than 600 regions of interest, the new model’s accuracy was 90%.
“Existing modalities are mainly based on the size and shape of the ovarian lesions, which do not provide an accurate diagnosis for earlier ovarian cancer and for risk assessment of large adnexal/ovarian lesions,” said Zhu, also a professor of radiology at the School of Medicine. “Photoacoustic imaging adds more functional information about vascular contrast from hemoglobin concentration and blood oxygen saturation.”
Yun Zou, a doctoral student in Zhu’s lab, developed the machine learning fusion model by combining an ultrasound neural network with a photoacoustic tomography neural network to perform ovarian lesion diagnosis. Cancerous lesions of the ovaries can present in several different morphologies from ultrasound. While some are solid, others have papillary projects inside cystic lesions, which makes them more difficult to diagnose. To improve the overall diagnosis capabilities of ultrasound, the teams added the total hemoglobin concentration and blood oxygenation saturation from photoacoustic imaging, both of which are biomarkers for cancerous ovarian tissue.
“Our results showed that the ultrasound-enhanced photoacoustic imaging fusion model reconstructed the target’s total hemoglobin and blood oxygen saturation maps more accurately than other methods and provided an improved diagnosis of ovarian cancers from benign lesions,” Zou said.













