New research headed by teams at the University of Texas MD Anderson Cancer Center and the Center for Cancer Research at the National Cancer Institute (NCI) suggest that a high-fiber diet may help some melanoma patients respond better to immunotherapy treatments by influencing the gut microbiome.
The study found that patients with melanoma who reported eating more fiber-rich foods when they began immunotherapy treatment survived longer without cancer growth than patients with insufficient dietary fiber intake. More specifically, among patients with advanced melanoma who underwent immune checkpoint blockade (ICB) immunotherapy, those who consumed at least 20 g a day of dietary fiber survived the longest without their disease progressing. In contrast, the use of probiotic supplements appeared to lessen the effectiveness of immune checkpoint blocker regimens. Parallel preclinical studies in mouse models supported findings from the observational study in human patients.
“Research from our team and others has shown that gut microbes impact response to immunotherapy treatment, but the role of diet and probiotic supplements has not been well studied,” said Jennifer Wargo, M.D., professor of genomic medicine and surgical oncology. “Our study sheds light on the potential effects of a patient’s diet and supplement use when starting treatment with immune checkpoint blockade. These results provide further support for clinical trials to modulate the microbiome with the goal of improving cancer outcomes using dietary and other strategies.”
Co-research led Giorgio Trinchieri, MD, chief of the Laboratory of Integrative Cancer Immunology in NCI’s Center for Cancer Research, further commented, “The data suggest that one can target the composition of the gut microbiota and affect the ability of the patient to respond to immunotherapy. Consuming a diet rich in fiber, like fruits, vegetables, and legumes, could improve your ability to respond to immunotherapy.”
Co-senior author Wargo, Trinchieri, and colleagues reported on their studies in Science, in a paper titled, “Dietary fiber and probiotics influence the gut microbiome and melanoma immunotherapy response.” Based on the findings, a clinical study is now underway to investigate how whole-food-based diets with varying fiber content affect the microbiome and immune response.
Immunotherapy with immune checkpoint blockers helps to restore the immune system’s natural ability to recognize and kill tumor cells. Immune checkpoint blockade has been transformative in melanoma, improving survival time in patients with advanced disease, sometimes by years. However, for many patients, immune checkpoint blockers fail to stop tumor growth. Several studies have suggested that the composition of the bacteria in the gut may influence the response to immunotherapy, the authors noted. “ … the influence of the gut microbiome on therapeutic response has now been demonstrated in numerous human cohorts and in preclinical models.” As Trinchieri pointed out, “The question is, can we change the composition of the type of bacteria in the gut and improve the ability of the patient to respond?”
The human gut microbiome is itself shaped by a wide variety of environmental exposures, including diet and medication use, and host genetics account for less than 10% of variation, the team continued. “However, whether factors such as dietary fiber intake and the use of commercially available probiotics affect immunotherapy responses in cancer patients remains unclear.”
In a previous study, Trinchieri together with a different group of collaborators, also showed that some people with melanoma who initially did not respond to treatment using an immune checkpoint blocker did respond after receiving a fecal transplant from a patient who had responded to the drug. The fecal transplant, they concluded, had introduced different gut bacteria that helped to make it easier for immune cells to invade and kill their tumors.
“Dietary fiber intake and use of probiotic supplements have also been shown to affect the composition of gut bacteria,” Trinchieri said. “More cancer patients are taking probiotic supplements in an effort to improve their gut health, but little is known about how probiotics—which basically change the ecology of the gut bacteria—impact immunotherapy response.” And interestingly, while the connection between fiber intake and immunotherapy response has not been clear, a recent study led by NCI Center for Cancer Research scientists showed that mice fed a diet rich in pectin, which is a fiber abundant in apples, were able to stave off tumor growth by activating immune cells and reprogramming the tumor microenvironment.
For the newly reported study, Trinchieri, Wargo, and collaborators looked at the composition of fecal microorganisms, dietary habits, and probiotic supplement use among patients who were being treated for advanced melanoma using immune checkpoint blockers. The study began with analyzing the gut microbiome profiles of 438 melanoma patients, 321 of whom had late-stage disease and were treated with systemic therapy, and 293 of whom had an evaluable response to treatment over follow-up. The majority of these patients (87%) received immune checkpoint blockade, most commonly PD-1 inhibitors. A total of 158 patients also completed a lifestyle survey of antibiotics and probiotics usage; of these, 128 completed a dietary questionnaire as they began immune checkpoint therapy.
The results showed that among the 128 patients whose dietary fiber intake was known, those who reported consuming at least 20 g of dietary fiber per day (an amount the researchers designated as “sufficient” for the purposes of this study) lived longer without their cancer progressing than those who consumed less dietary fiber. Every 5 g increase in daily dietary fiber intake corresponded to a 30% lower risk of disease progression.
When the patients were further grouped according to high- or low-fiber diet and commercially available probiotic supplement use, response to immunotherapy was seen in 18 of 22 patients (82%) who reported both sufficient fiber intake and no probiotic use, compared to the response seen in 60 of 101 (59%) patients who either reported insufficient fiber intake or probiotic use. Response was defined as complete or partial complete or partial tumor shrinkage or stable disease for at least six months. Probiotic use alone was not associated with a significant difference in progression-free survival or odds of response to immunotherapy.
Nearly one-third of the patients reported they had taken a probiotic supplement within the past month. And although the researchers noted that the small sample size and variety of probiotics used by the patients made it difficult to draw definitive conclusions about the association between probiotic use and response to immune checkpoint blockers, they did observe that patients who consumed the highest levels of dietary fiber with no probiotic use survived the longest. “Together, these data have important implications,” they noted. “We show that dietary fiber and probiotic use, factors known to affect the gut microbiome, are associated with differential outcomes to ICB.”
The research team reinforced their prior findings, which showed a higher abundance of Ruminococcaceae and Faecalibacterium prausnitzii—well-known and potentially beneficial bacteria involved in the digestion of fiber or starch—in patients who responded to immunotherapy. “ … patients whose cancer responded to immunotherapy had a greater abundance of Ruminococcaceae bacteria in their gut microbiota compared with those who did not respond to therapy,” Trinchieri commented. In contrast to the previous findings, however, overall diversity of gut bacteria was not associated with response to immunotherapy, potentially due to the larger size of this patient cohort.
“Dietary fiber is important for gut health, just as it’s important for overall health, and the two things are very tightly intertwined,” said co-senior author Carrie Daniel-MacDougall, PhD, associate professor of epidemiology. “In this study, we saw that dietary fiber also may be important to cancer treatment, which brings us to a point where we can design interventional studies to answer the questions that patients really want answered: ‘Does what I eat now matter and could it impact my treatment outcome?’ We’re united in working to find answers for our patients.”
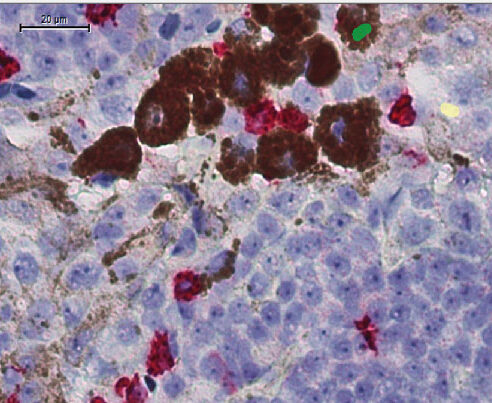
The researchers also looked at the impact of dietary fiber on the response to ICB immunotherapy using anti-PD-1 drugs in mouse models of melanoma. To mimic the different diets in the melanoma patients, they fed mice either a fiber-rich or a low-fiber diet, injected the mice with melanoma cells, and then treated the mice using an anti-PD-1 immunotherapy. In multiple models, probiotic use was associated with impaired response to immune checkpoint blockade, and with larger tumors, lower gut microbiome diversity and less cytotoxic T cells in the tumor microenvironment. A high-fiber diet was associated with slower tumor growth and significantly higher frequency of CD4+ T cells in the preclinical models treated using PD-1 inhibitors. “Immune profiling by flow cytometry of tumors in treated mice revealed a significantly higher frequency of CD4+ T cells overall (and those expressing PD-1) in the tumors of mice on high- versus low-fiber diets,” the investigators noted. “Profiling of the gut microbiome revealed significant differences in the community structure of mice fed fiber-rich versus fiber-poor diets and taxonomic differences between the groups.”
The researchers repeated the experiments in germ-free mice that had no bacteria in their guts. “In germ-free mice, the diet made no difference in the immunotherapy response,” Trinchieri said. “That suggests that the diet is affecting the response to immune checkpoint therapy by changing the composition of the gut microbiota.” Trinchieri further noted that one possible mechanism through which dietary fiber exerts its beneficial effect is by increasing the types of bacteria in the gut, such as Ruminococcaceae, that produce high levels of certain short-chain fatty acids that have an antitumor effect.
“We did see an increase in one of these short-chain fatty acids, propionate, in mice that were fed a high-fiber diet,” Trinchieri said. As the authors wrote, “Stool metabolomic profiling also revealed significantly higher levels of the short chain fatty acid (SCFA) propionate in mice receiving a fiber-rich diet, although no significant differences were noted in SCFA levels as a whole.”
“The impact of dietary fiber and probiotics on the gut microbiota is only part of the bigger picture,” Trinchieri cautioned. “Many factors can affect the ability of a patient with melanoma to respond to immunotherapy. However, from these data, the microbiota seems to be one of the dominant factors. The data also suggest that it’s probably better for people with cancer receiving immunotherapy not to use commercially available probiotics.”
The authors acknowledged that causality can’t be addressed from the observational human cohort. However, they pointed out, “Our preclinical models support the hypothesis that dietary fiber and probiotics modulate the microbiome ad that antitumor immunity is impaired in mice receiving a low-fiber diet ad in those receiving probiotics—with suppression of intratumoral IFN- γ T cell responses in both cases.” Moreover, they suggested, while their findings suggest that undirected use of commercially available probiotics may be harmful in the context of ICB therapy, “… further study of rationally designed and targeted probiotics or bacterial consortia is warranted on the basis of promising early data of this approach.”
And as they further concluded, “In light of these collective results, dietary habits and probiotic supplement use should be considered in patients receiving ICB and in efforts to modulate the gut microbiota. These factors should be more thoughtfully evaluated in strategies to improve cancer outcomes.”
Based on the early study findings, a randomized clinical trial (NCT04645680), led by co-first author Jennifer McQuade, M.D., assistant professor of melanoma medical oncology, will examine how whole-food-based diets with varying fiber content affect the microbiome and immune response. The study is currently enrolling patients with stage III–IV melanoma who are receiving immunotherapy.
“Our research teams within the Program for Innovative Microbiome and Translational Research (PRIME-TR) and Bionutrition Research Core at MD Anderson are collectively working to transform cancer therapy by modifying the microbiome,” Wargo said. “We’re grateful to the patients and families who have participated in our research and are hopeful that this work will ultimately provide evidence-based guidance to help patients take control of their own diets to improve their odds against cancer.”













