A research collaboration led by Ben Gurion University has developed molecular tweezers to combat antibiotic resistant bacteria by breaking up biofilm formation.
‘Molecular tweezers’ are molecules designed with open gaps that can bind to other molecules in a tweezer-like fashion. They are still a relatively new concept, but have potential for a number of medical applications for example to bind to and break down amyloid plaques.
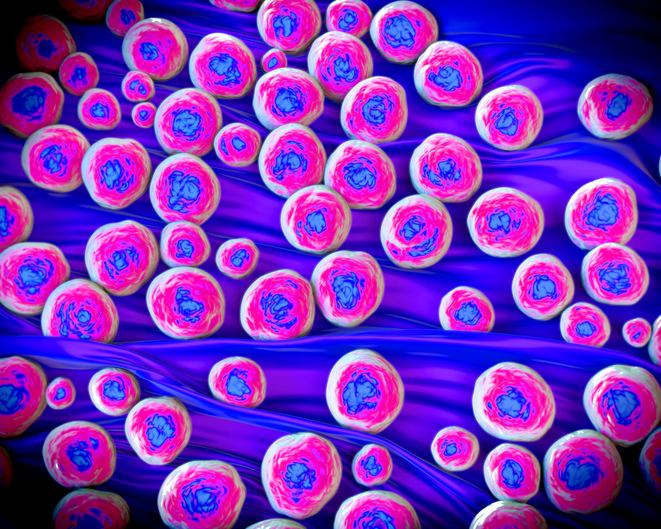
Staphylococcus aureus bacteria are commonly found on the skin and in human airways and is normally a harmless commensal bacterium. However, it can become pathogenic and is a common cause of potentially life-threatening hospital-acquired infections such as pneumonia, sepsis and endocarditis, among others.
If S. aureus forms biofilms these can be very hard to treat and are often antibiotic resistant – as in methicillin-resistant S. aureus (MRSA) cases. To combat this problem, Raz Jelinek, Ph.D., a professor at Ben Gurion University of the Negev in Israel and colleagues tested the ability of three molecular tweezers known as CLR01, CLR03 and CLR05, previously found to disrupt amyloid self-assembly, to disrupt S. aureus biofilm formation.
In addition to other researchers at Ben Gurion, scientists from the University of Duisburg-Essen in Germany and Rensselaer Polytechnic Institute and UCLA in the U.S. also took part in the project and were authors on the paper describing the work published in Cell Chemical Biology.
While amyloid plaques are most well-known for their role in Alzheimer’s disease and other neurodegenerative disorders, many bacterial biofilms (including those made by S. aureus) also contain proteins that form amyloid-like fibrils and plaques.
The research team found that the tweezer molecule they used was able to disrupt and breakdown the S. aureus biofilms. In particular, CLR01 disrupted phenol-soluble modulin α1 – a structural amyloid peptide that S. aureus uses to build biofilms. CLR05 has a slightly different mechanism of action, but seemed to disrupt biofilm formation even more strongly. In contrast, CLR03 was not able to disrupt biofilm formation.
“The tweezers are just like your home tweezers but a million times smaller, and instead of plucking hairs they attack fibers of the bacteria’s biofilm. By doing that they break the biofilm, making it more vulnerable to human immune defenses and external substances that are used against bacteria like antibiotics,” said Jelinek in a press statement.
“We found that binding the tweezers to the biofilm disrupts its protective capabilities. Consequently, the bacterial pathogens become, less virulent to the human body, and, more vulnerable to elimination by the immune system.”
An important aspect of the mechanism of action of the molecular tweezers is that they disrupt the biofilm formation, without killing off all the bacteria. This can be important to help prevent antibiotic resistance and also to help maintain a healthy microbiome by not killing off helpful commensal bacteria.
“Our discovery prevents infection without building up antibiotic resistance,” said Jelinek. “This breakthrough may open up new ways to fight antibiotic-resistant bacteria.”











