Scientists at Mount Sinai’s Icahn School of Medicine have uncovered new molecular drivers of Parkinson’s disease using multiscale gene network analysis (MGNA). The team was also able to determine how these molecular drivers may point to potential new treatments. Their results were published this week in Nature Communications.
“This study offers a novel approach to understanding the majority of cases of Parkinson’s,” said Bin Zhang, Ph.D., one of the authors and Professor of Genetics and Genomic Sciences at the Icahn Institute for Data Science and Genomic Technology and Director of the Mount Sinai Center for Transformative Disease Modeling at the Icahn School of Medicine at Mount Sinai. “The strategy not only reveals new drivers, but it also elucidates the functional context of the known Parkinson’s disease risk factor genes.”
Parkinson’s disease affects one to two people out of 1000, with prevalence increasing with age. While some cases of Parkinson’s appear to be directly caused by genetic mutations, such cases are rare. Approximately 80 percent of cases have no known cause. There are some genes that appear to slightly increase an individual’s risk of developing the disease, but their biological impact remains unclear. As a result, there is great interest in unravelling the causes of this disease.
“This multiscale network analysis approach is a powerful way to dissect the molecular mechanisms of complex diseases like Alzheimer’s,” said Suzana Petanceska, Ph.D., program director of the AMP-AD Target Discovery program at the National Institute on Aging (NIA), which co-funded the study. “It is exciting to see that AMP-AD can provide new mechanistic insights to Parkinson’s disease that could lead to new therapeutic opportunities.”
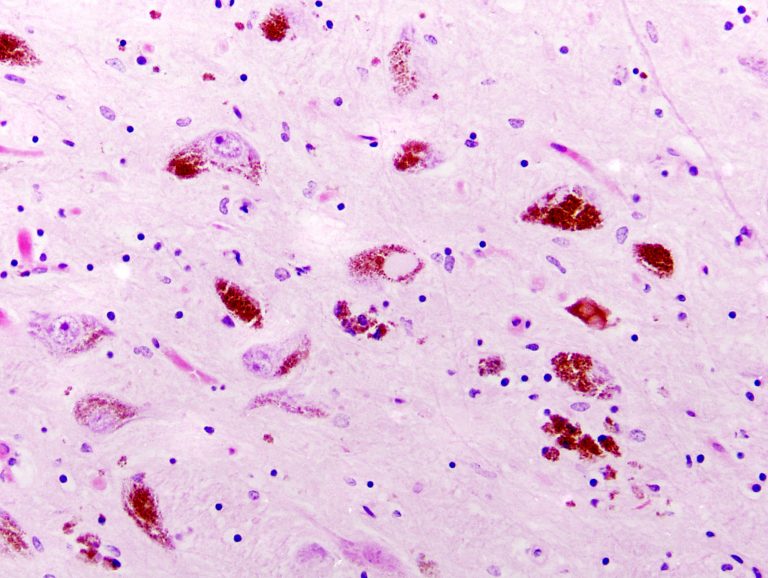
The researchers combined data from eight different studies that included postmortem analyses of the substantia nigra—the part of the brain most affected by Parkinson’s disease. This gave the team a dataset from a total of 83 patients, which they then compared to 70 controls who did not have Parkinson’s. Applying MGNA to the combined data set, the scientists identified a number of key regulators of the gene networks that had never before been associated with the disease.
Applying MGNA to the combined data set, the scientists identified a number of key regulators of the gene networks that had never before been associated with the disease.
Next, they teamed up with Zhenyu Yue, Ph.D., Professor of Neurology and Neuroscience at the Icahn School of Medicine and the Director of Basic and Translational Research in Movement Disorders—whose work is supported by NIH Udall Centers of Excellence for Parkinson’s Disease Research—to experimentally validate the findings in mice. They chose to test the effects of STMN2, a gene that the analysis identified as a key regulator of the Parkinson’s molecular network. The gene is normally expressed in neurons that produce dopamine, a neurotransmitter that is depleted in the substantia nigra of Parkinson’s patients.
To test its influence on Parkinson’s disease, Yue and his team knocked down the STMN2 gene in the substantia nigra of the mice. RNA sequencing showed that reduction of STMN2 led to upregulation of nine genes previously associated with the disease. The mice developed Parkinson’s-like pathologies such as degeneration of dopaminergic neurons in the substantia nigra and an increase in the concentration of the toxic, modified α-synuclein protein, both of which are considered hallmarks of the disease. Additionally, the mice struggled with motor tasks such as maintaining balance on a rod, indicative of the disruption of their motor function control.
While 83 patients is still a relatively small number, and the results should be validated in larger studies, “The work opens up a new avenue for studying the disease,” said Yue. “The new genes we identified suggest that new pathways should be considered as potential targets for drug development, particularly for idiopathic Parkinson’s cases.”













