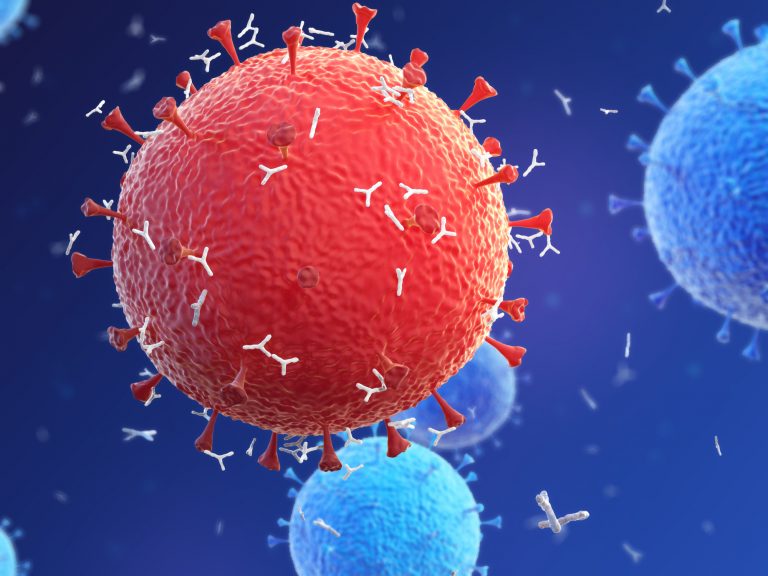
A U.K.-based study using multi-omic techniques reveals that asymptomatic and mildly affected patients infected with the SARS-CoV-2 virus have high levels of immune cells—antibody-producing B cells and T helper cells—that are not seen in those with more severe COVID-19.
Notably, the research showed that patients with severe disease had not only lost most of these helpful immune cells, but also had high levels of monocytes, T-killer cells and platelet-producing cells, which increase inflammation in the body and promote the formation of blood clots.
“This is one of the only studies of its kind that looks at samples collected from asymptomatic people, which helps us start to understand why some people react differently to COVID-19 infection. It could also explain symptoms such as lung inflammation and blood clots,” said Muzlifah Haniffa, M.D., Ph.D., a professor at Newcastle University and researcher at the Wellcome Sanger Institute in Hinxton, who co-led the study.
“The immune system is made up of lots of different groups of cells, similar to the way an orchestra is made up of different groups of instruments, and in order to understand the coordinated immune response, you have to look at these immune cells together.”
The study, which is published in the journal Nature Medicine, involved single-cell transcriptome and surface proteome analysis of over 780,000 immune cells taken from 130 patients infected with SARS-CoV-2. The researchers also analyzed cell surface T and B lymphocyte antigen receptors on the cells.
The 102 COVID-19 patients included in the study had a range of disease severity from asymptomatic to severe or critical disease. The other participants were either healthy or hospitalized patients without COVID-19. The patients were recruited in Cambridge, London and Newcastle in the UK.
In asymptomatic people infected with the virus, the team found higher than normal levels of antibody-producing B cells found in mucus producing tissues such as the nasal passages. They also saw high levels of these cells and T helper cells in patients with mild-moderate infection.
The levels of these helpful immune cells dropped significantly in patients with more severe disease, which might at least partly explain why their symptoms are more severe. Individuals with more severe disease also had rapid increases in inflammatory cells – monocytes and T killer cells—and platelet-producing cells, which likely underlies the excessive immune reaction and frequent blood clots seen in more severely affected COVID-19 patients.
More research is required to find out why the virus stimulates different immune responses in different people and also how the knowledge of these differences could help design future treatments or diagnostics. However, this study goes some way to explaining the differences seen in people infected with SARS-CoV-2.
This research is part of the Human Cell Atlas, an international collaboration to comprehensively map all human cells on a molecular level.
“This is a great example of using the Human Cell Atlas to understand COVID-19 and identify which of our cells are critical for infection and treatment. This information can be used to better understand why different people react to coronavirus in different ways. The data is openly accessible and can provide a basis for developing potential new therapies, to reduce the spread of the virus, or to protect those who start to develop severe disease,” commented Sarah Teichmann, Ph.D., senior author from the Wellcome Sanger Institute and co-chair of the Human Cell Atlas Organizing Committee.













