A new method of irradiating pancreatic tumors combined with chemotherapy drugs tested by researchers at Duke University has shown promise in mouse models, according to new research published in Nature Biomedical Engineering.
The researchers say the new approach eliminated tumors in 80% of mice across several model types. The new approach may pave the way for more treatment options for pancreatic cancer.
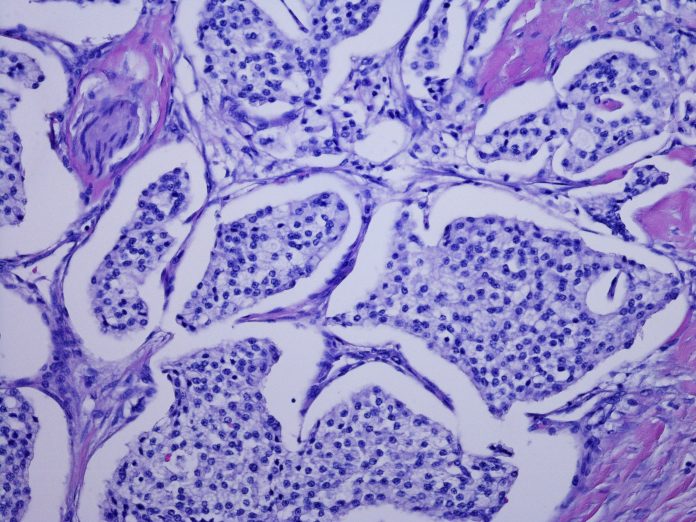
“Locally advanced pancreatic tumors are highly resistant to conventional radiochemotherapy,” wrote the researchers. “Here we show that such resistance can be surmounted by an injectable depot of thermally responsive elastin-like polypeptide (ELP) conjugated with iodine-131 radionuclides (131I-ELP) when combined with systemically delivered nanoparticle albumin-bound paclitaxel. This combination therapy induced complete tumor regressions in diverse subcutaneous and orthotopic mouse models of locoregional pancreatic tumors.”
The novel treatment implants radioactive iodine-131 directly into the tumor within a gel-like depot that protects healthy tissue and is absorbed by the body after the radiation fades away.
“We did a deep dive through over 1,100 treatments across preclinical models and never found results where the tumors shrank away and disappeared like ours did,” said Jeff Schaal, who conducted the research during his PhD in the laboratory of Ashutosh Chilkoti, PhD, the Alan L. Kaganov distinguished professor of biomedical engineering at Duke. “When the rest of the literature is saying that what we’re seeing doesn’t happen, that’s when we knew we had something extremely interesting.”
The current leading treatment combines chemotherapy with a beam of radiation targeted at the tumor. This approach, however, is ineffective unless a certain threshold of radiation reaches the tumor.
Another method researchers have tried involves implanting a radioactive sample encased in titanium directly within the tumor. However, because titanium blocks all radiation other than gamma rays, it can only remain within the body for a short period of time before damage to surrounding tissue begins.
“There’s just no good way to treat pancreatic cancer right now,” explained Schaal, who is now director of research at Cereius, a Durham, NC, biotechnology startup.
Schaal decided to try a similar implantation method using a substance made of ELPs. When injected into a tumor along with a radioactive element, the ELPs form a small depot encasing radioactive atoms. The researchers decided to use iodine-131 because doctors have used it widely in medical treatments for decades and its biological effects are well understood.
Schaal and his collaborators in the Chilkoti laboratory tested the new treatment in concert with paclitaxel, a commonly used chemotherapy drug, to treat various mouse models of pancreatic cancer.
The researchers tested their approach on mice with cancers just under their skin created by several different mutations known to occur in pancreatic cancer. They also tested it on mice that had tumors within the pancreas.
Overall, the tests saw a 100% response rate across all models, with the tumors being completely eliminated in three-quarters of the models about 80% of the time. The tests also revealed no immediately obvious side effects beyond what is caused by chemotherapy alone.
“We think the constant radiation allows the drugs to interact with its effects more strongly than external beam therapy allows,” Schaal said. “That makes us think that this approach might actually work better than external beam therapy for many other cancers, too.”
Further studies are needed before the treatment is seen in the clinic. The next step for researchers is large animal trials, where they will need to show that the technique can be accurately done with the existing clinical tools and endoscopy techniques that doctors are already trained on. If successful, they look toward a Phase I clinical trial in humans.
“My lab has been working on developing new cancer treatments for close to 20 years, and this work is perhaps the most exciting we have done in terms of its potential impact, as late-stage pancreatic cancer is impossible to treat and is invariably fatal,” Chilkoti said. “Pancreatic cancer patients deserve better treatment options than are currently available, and I am deeply committed to taking this all the way into the clinic.”













