Optical coherence tomography (OCT) and machine learning have been combined to develop a colorectal cancer imaging tool that may one day improve diagnostics endoscopy procedures.
In a recent study, the technique provided more information about an abnormality than surface-level, white-light images currently used by physicians. Shuying Li, a biomedical engineering PhD student working in the lab of Quing Zhu, at the McKelvey School of Engineering at Washington University in St. Louis, used the imaging data to train a machine learning algorithm to differentiate between “normal” and “cancerous” tissue. The combined system allowed them to detect and classify cancerous tissue samples with a 93% diagnostic accuracy.
The results were published in the Journal of Biophotonics. Hongbo Luo, a PhD student in Zhu’s lab, led the work.
According to the American Cancer Society, overall, the lifetime risk of developing colorectal cancer is about 1-in-23 (4.3%) for men and 1-in-25 (4.0%) for women. Cancer of the colon and rectum is the second most common malignancy diagnosed globally and represents the second leading cause of cancer mortality worldwide.
An estimated 5% to 10% of colon cancer is hereditary. The major hereditary colon cancer syndromes being Lynch syndrome (Hereditary Non-Polyposis Colorectal Cancer or HNPCC) and Familial Adenomatous Polyposis (FAP). Other genes and proteins have also been implicated in colon cancer risk, including MLL1.
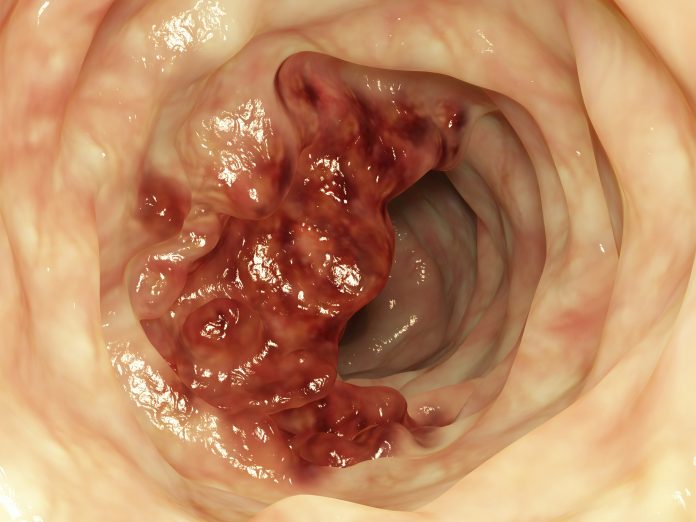
Screening for colon cancer currently relies on human visual inspection of tissue during a colonoscopy procedure, which does not detect and diagnose subsurface lesions. Zhu pointed out to Inside Precision Medicine, that “The vast majority of human colorectal cancers arise from polyps which have different risk categories and are more complex than rat models.”
OCT is an emerging imaging technique that strives to obtain 3-dimensional “optical biopsies” of biological samples with high resolution. In prior work, several research groups have reported that OCT, an established high resolution imaging modality, could overcome the shortcoming of traditional camera endoscopy in the upper gastrointestinal tract or large intestine.
This team designed a convolutional neural network to capture the structure patterns in human colon OCT images. The network was trained and tested using around 26,000 OCT images acquired from 20 tumor areas, 16 benign areas, and 6 other abnormal areas.
The trained network successfully detected patterns that identify normal and neoplastic colorectal tissue. Experimental diagnoses predicted by the PR-OCT system were compared to the known histologic findings and quantitatively evaluated. A sensitivity of 100% and specificity of 99.7% was reached.
An endoscopy OCT essentially shines a light in the colon to help a clinician see deeper to visualize and diagnose abnormalities. By collaborating with physicians at Washington University School of Medicine and with Chao Zhou, associate professor of biomedical engineering, the team developed a small OCT catheter. It uses a longer wavelength of light, to penetrate 1-2 mm into the tissue samples.
As Zhu further explained, while also referencing an earlier paper from her group, “We have developed our unique pattern recognition neural networks trained from the data we collected from human colorectal tissue samples. Our neural networks identify features of normal colorectal tissue OCT images and distinguish cancers based on the abnormal patterns of OCT images.”
She noted out that the current technique includes miniature OCT imaging catheter development and scanning assembly design that can be integrated into clinical colonoscopy.













