A team of researchers at the Swiss Federal Institute of Technology Lausanne (EPFL) have identified protein cathepsin S. (CTSS) as a mechanism used by Non-Hodgkin lymphoma (NHL) to evade the immune system. This discovery provides a future target for clinical NHL treatment.
A scientific team led by Elisa Oricchio, Ph.D., found that certain patients with NHL have a mutated and over-activated form of CTSS. These mutations can induce a tumor-promoting immune microenvironment in certain types of lymphoma. The normal version of this protein is responsible for cutting other proteins into small fragments, and then displaying fragments of those proteins on the surface of tumor cells. These fragments mediate communications between cancer and immune cells.
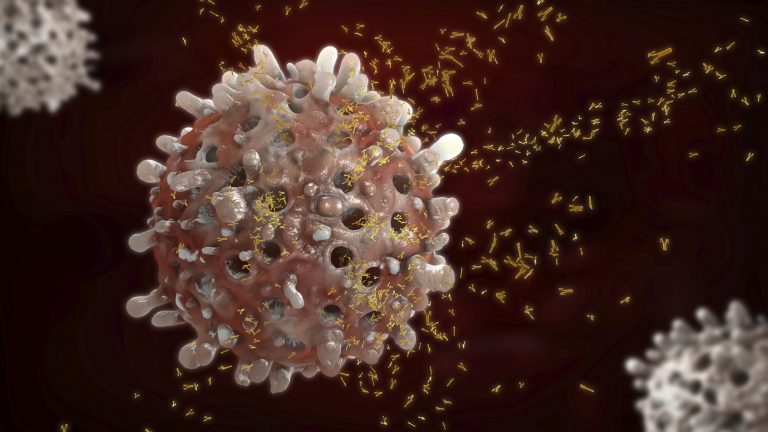
NHL makes up a unique group of cancers which originate in lymph nodes and affects B cells, a type of immune cell. In patients with NHL, B cells grow and replicate out of control, creating tumors in the lymph nodes, spleen, and/or other tissues associated with the blood. According to the American Cancer Society, about 80,000 people will be diagnosed with NHL in 2020, and 20,000 will die of it.
Immunotherapy is one of the most promising treatment for cancer patients, and is rather new. Unlike radiation therapy or chemotherapy, immunotherapy directs the patient’s own immune system to attack and eliminate tumor cells. However, oftentimes tumor cells will then mutate to evade immune system detection or even exploit interactions with immune cells to facilitate their own growth. Also, it is increasingly recognized in research that tumor cells must facilitate and depend on interactions with non-malignant cells of the tumor microenvironment in order to survive. Understanding that relationship will be key in eliminating tumor cells in patients.
“When cathepsin S is active, cancer cells interact with immune cells called CD4+ T-cells, which help the tumor to grow, while they maintain social distance with CD8+ T-cells, which would attack and kill the tumor,” explains Elie Dheilly, one of the lead authors of the study.
The identification of this duplicitous relationship between cancer cells and T-cells prompted the researchers to study cancer cells which had been genetically modified to no longer express CTSS, so that they might understand how tumor growth would be affected.
They discovered that Inhibiting CTSS reduced tumor growth by inverting the communication with T-cells: CD8+ T-cells were now attacking the tumor, while CD4+ T-cells were kept at bay. The researchers believe this is occurring by inducing “antigen diversification”, where the cell is generating a different population of fragments to help T-cells to identify and kill tumor cells.
“We think that cathepsin S could represent an important therapeutic target,” says Oricchio. “Inducing antigen diversification is an attractive therapeutic strategy to increase tumor immunogenicity and enhance response to immunotherapies in lymphoma, but possibly also in other tumor types.”
The researchers on this project studied CTSS in two forms; in mouse models and in clinical patients. Tumors with hyperactive CTSS showed increased CD4+ T cell infiltration and pro-inflammatory cytokine perturbation in both the mouse model and in human subjects, but interestingly, in mice, a CTSS-induced immune microenvironment promoted tumor growth, while in clinic, patients with hyperactive CTSS lymphoma had better treatment outcomes with standard immunotherapies. This indicates that immunosuppressive regimens target both lymphoma cells and the tumor-promoting immune microenvironment.
Based on the finding of this study, the researchers propose a model in which a mutated CTSS with hyperactivity induces and activates a CD4+ T cell enriched immune microenvironment, which ultimately promotes tumor growth. Although the cellular adaptive immune system is often thought of in the context of immune surveillance and anti-tumor responses, the concept of CD4+ T cells supporting the growth of human lymphoma cells dates back to the 1990s.
In addition to deducing the cellular interactions that occur in this CTSS model, during the study co-lead author Elena Battistello developed a new imaging technique to specifically measure the activity of CTSS. Using this technique, Oricchio and her team have identified and further developed new inhibitors (patent application filed) that could be used to improve the treatment of patients diagnosed with NHL.













