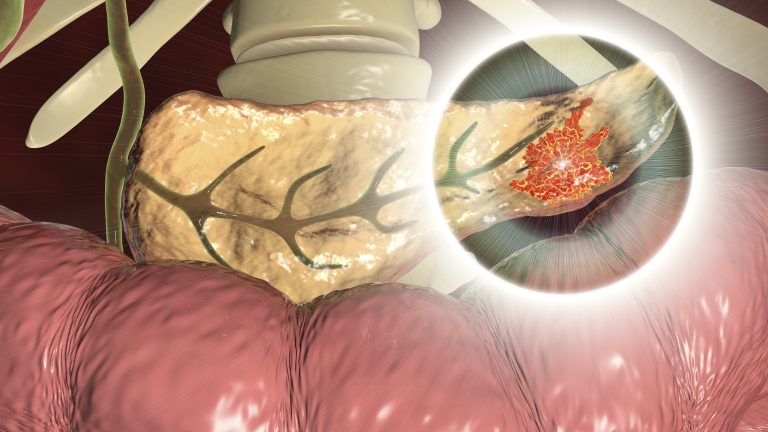
A mouse study reveals mesothelial-derived, scar-like cells make up a large portion of malignant pancreatic tumors and shield these cancers from immune attack, according to research from UT Southwestern (UTSW).
“Recent studies have identified a unique cancer-associated fibroblast (CAF) population termed antigen-presenting CAFs (apCAFs), characterized by the expression of major histocompatibility complex class II molecules, suggesting a function in regulating tumor immunity,” the researchers wrote. “Here, by integrating multiple single-cell RNA-sequencing studies and performing robust lineage-tracing assays, we find that apCAFs are derived from mesothelial cells.”
Their findings, published in the journal Cancer Cell, could offer a new strategy to fight pancreatic cancer. “By targeting antigen-presenting cancer-associated fibroblasts, we might someday be able significantly to enhance the activity of immune therapy in pancreatic cancer patients,” said Huocong Huang, instructor of surgery at UTSW. Huang co-led the study with Rolf Brekken, professor of surgery, pharmacology, a principal investigator at UTSW’s Hamon Center for Therapeutic Oncology Research, and is a member of the Harold C. Simmons Comprehensive Cancer Center.
Researchers have long known that cells called CAFs make up a significant portion of pancreatic tumors. Although scientists have considered these pancreatic CAFs to be a uniform population, Huang explained, he and his colleagues in the Brekken lab showed in a 2019 study that these cells fall into three categories. One of these is a subtype known as apCAFs, which interact with immune cells by displaying proteins called antigens on their surface.
To determine how apCAFs contribute to PDA progression, Huang, Brekken, and their colleagues used a technique known as lineage tracing to learn how these cells arise as a normal pancreas develops cancer. Their findings showed that apCAFs originate from mesothelial cells, which form a protective membrane that lines organs, body cavities, and tissues.
Further experiments showed that the antigens on the surface of apCAFs could convert T cells into a subset known as regulatory T cells (Tregs). When the researchers dosed mice carrying pancreatic tumors with antibodies against mesothelin, a protein unique to mesothelial cells, the conversion to Tregs was blocked, leaving tumors more vulnerable to an anti-tumor immune response.
Further studies are needed. However, a similar strategy may one day be used to treat PDA in humans by administering anti-mesothelin antibodies in combination with immunotherapies that stimulate the immune system to fight cancers.













