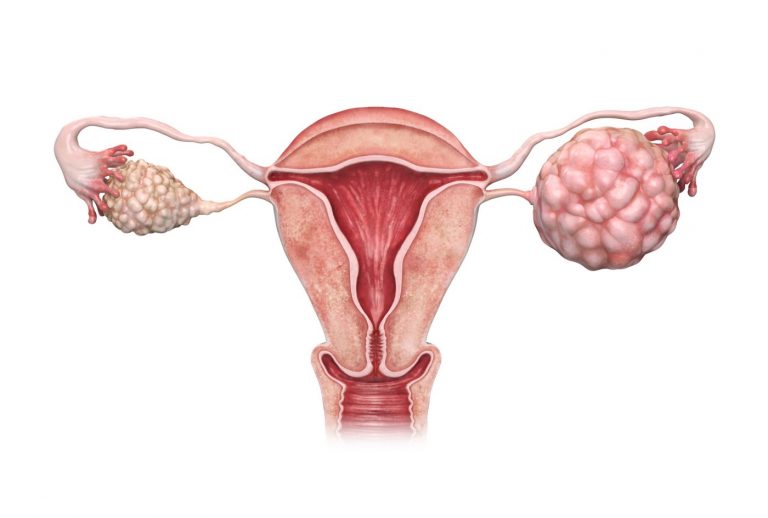
Once ovarian cancer cells slough off from their site of origin, they tend to find a new home in tissues with high fat content. Now, researchers have shown that those ovarian cancer cells use fats as an energy source. At the heart of the transition to fatty acid metabolism is the enzyme Carnitine Palmitoyltransferase 1A (CPT1A), which may control how much fat these cancer cells can burn. In turn, a treatment that limits these cells’ access to CPT1A may starve them of the resources they need to spread.
A group of researchers from Colorado have collaborated to gain a better understanding of the role of CPT1A on the spread of ovarian cancer cells, showing that they may be necessary for ovarian cancer dissemination, chemo-resistance. Not only that, but they are working to bring this strategy to patients who need it.
The research is published in the paper, “Targeting fatty acid oxidation to promote anoikis and inhibit ovarian cancer progression” in Molecular Cancer Research.
“When they break off, they metabolically shift to use fats more—it allows these cells to survive and then they seek out or are able to colonize fatty tissue,” said Benjamin Bitler, Ph.D., assistant professor in the division of reproductive sciences at the University of Colorado (CU) School of Medicine department of obstetrics & gynecology. “It looked like CPT1A was the rate-limiting step in their ability to do this,” he added.
Interestingly, Bitler was in a serendipitous position to delve deeper into the role of CPT1A in ovarian cancer dissemination. That’s because one of the world’s experts on this enzyme happens to work on the same campus. The laboratory of Isabel Schlaepfer, Ph.D., had been working on the role of CPT1A in the progression of prostate cancer.
“With Isabel’s lab, we were able to demonstrate that, yes, the cells become more dependent on fatty acids to survive the attachment-free environment,” Bitler said. The team examined the contribution of fatty acid oxidation (FAO) in supporting anoikis (apoptosis triggered by cell detachment) resistance and showed that by adding fatty acids to a model of ovarian cancer cells in suspension, they could prevent these cells from dying.
Likewise, the group was also able to show that by knocking down CPT1A, they could keep ovarian cancer cells from spreading in cell culture studies and slow the spread of human cancer cells grown in mouse models.
“It didn’t completely abolish ovarian cancer cells’ capacity to go to fat-rich sites, but it reduced it pretty dramatically,” he said.
The group then sought out a potential new treatment option, based on this research.
“There’s a drug called etomoxir that inhibits CPT1A and has been tested as a preventative for congestive heart failure,” Bitler said. Clinical trials of preventive medicines have a very low tolerance for side-effects, and in the case of etomoxir with congestive heart failure, the risks outweighed the benefits. But in the context of treating cancer, Bitler suggested that the drug’s risk would be well within (and even much less than) risks of existing medicines.
The authors wrote that, “targeting FAO in high-grade serous ovarian cancer (HGSOC) to promote anoikis and attenuate dissemination is a potential approach to promote a more durable anti-tumor response and improve patient outcomes.”
“We are working with Brad [Corr] to move forward with this. The question is where exactly to put etomoxir with respect to patient treatment,” Bitler said. He explained that a major issue in the treatment of ovarian cancer is the disease’s ability to resist chemotherapy. “The cells we’ve been studying resist cell death because they need to disseminate. Avoiding cell death is at the heart of chemo-resistance as well,” he added.













