A high-speed 3D microscope known as MediSCAPE, developed by engineers at Columbia University, can image living tissues in real time making biopsies unnecessary.
Tissue biopsies, where a small section of tissue is removed from the body for further analysis, are commonly used for diagnosis of a number of different conditions, for example, to assess whether a tumor is cancerous. However, these processes take time and can be painful for patients.
“The way that biopsy samples are processed hasn’t changed in 100 years, they are cut out, fixed, embedded, sliced, stained with dyes, positioned on a glass slide, and viewed by a pathologist using a simple microscope. This is why it can take days to hear news back about your diagnosis after a biopsy,” says Elizabeth Hillman, professor of biomedical engineering and radiology at Columbia University and senior author of the study in Nature Biomedical Engineering.
Hillman and colleagues have been working on a type of microscope that is able to capture 3D images of tissue while still in the body. Called SCAPE (for Swept Confocally Aligned Planar Excitation microscopy) the microscope allows different 3D views of tissues in real time.
“Such a technology could give a doctor real-time feedback about what type of tissue they are looking at without the long wait,” she explains. “This instant answer would let them make informed decisions about how best to cut out a tumor and ensure there is none left behind.”
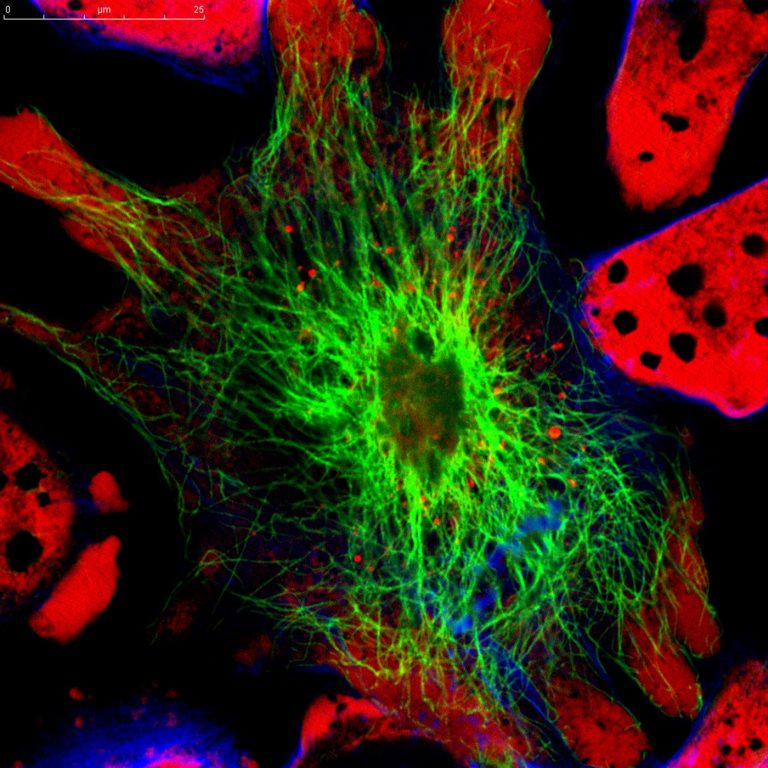
Starting with mouse kidney the team found the MediSCAPE machine was able to accurately visualize mouse kidney without adding any dyes to the tissue. “Everything we saw was natural fluorescence in the tissue that is usually too weak to see. Our microscope is so efficient that we could see these weak signals well, even though we were also imaging whole 3D volumes at speeds fast enough to rove around in real time, scanning different areas of the tissue as if we were holding a flashlight,” said Kripa Patel, a recent PhD graduate from the Hillman lab and first author of the study.
The machine allows ‘roving’ image acquisition, which allows motion such as blood flow to be imaged and images can be ‘stitched’ together to create a larger image.
“Understanding whether tissues are staying healthy and getting good blood supply during surgical procedures is really important,” says Hillman. “We also realized that if we don’t have to remove (and kill) tissues to look at them, we can find many more uses for MediSCAPE, even to answer simple questions such as ‘what tissue is this?’ or to navigate around precious nerves. Both of these applications are really important for robotic and laparoscopic surgeries where surgeons are more limited in their ability to identify and interact with tissues directly.”
One initial problem the engineers encountered was that the original machine is too large for regular use in a standard operating room. Hillman and colleagues created a smaller version that would be better suited to this task that had near equivalent accuracy on testing.
Following on from successful initial testing in mice and humans the engineers are now planning to commercialize the imaging technology and apply for FDA approval.
“The system is compact, relatively low cost and uses affordable, visible, continuous wave laser light sources (488nm and 637nm), with illumination levels equivalent to US FDA-approved confocal microendoscopy,” write the authors.
“This work shows the potential of MediSCAPE to become a rapid and low-cost alternative to conventional histopathology. Moreover, by providing real-time intraoperative feedback, MediSCAPE could enable closed-loop treatment decisions, including iterative assessment of surgical margins and more comprehensive surveillance of large tissue areas to guide biopsy site selection without the need to permanently damage or remove tissues that could otherwise be conserved.”













