A team of scientists from Singapore have demonstrated the critical role played by a transporter protein, Mfsd2a, in regulating the myelin sheath—the protective covering of nerves in the brain. The findings are reported by investigators at Duke-NUS Medical School and the National University of Singapore in the Journal of Clinical Investigation and could provide a pathway to help reduced the impacts of aging on the brain.
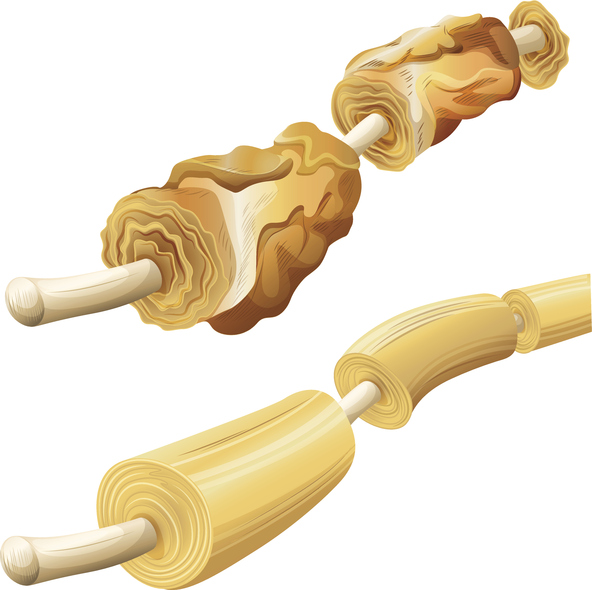
Myelin sheaths are an insulating covering of nerves which allow the proper conduction of electrical signals in the brain. Damaged myelin sheaths affect the ability of these nerves to function, resulting in neurological disorders. Myelin sheaths are known to naturally degenerate over time, which is the reason elderly people exhibit a loss of mental and physical functioning.
“Loss of myelin sheaths occurs during the normal aging process and in neurological diseases, such as multiple sclerosis and Alzheimer’s disease,” said Sengottuvel Vetrivel, PhD, senior research fellow with Duke-NUS’ Cardiovascular & Metabolic Disorders (CVMD) Program and the study’s lead investigator. “Developing therapies to improve myelination—the formation of the myelin sheath—in aging and disease is of great importance to ease any difficulties caused by declining myelination.”
In this new research, the team set out to better understand the role that Mfsd2a plays in the myelination process in the brain. The protein transports a lipid called lysophosphatidylcholine (LPC) and contains an omega-3 fatty acid. Previous research has shown that defects in the Mfsd2a gene lead to significantly reduced myelination and the birth defect microencephaly.
In preclinical models, the research team showed that removing Mfsd2a from precursor cells that mature into myelin-producing cells (oligodendrocytes) in the brain led to deficient myelin formation after birth. Digging deeper via the use of single-cell sequencing the investigators found that the absence of Mfsd2a caused a reduction in the pool of fatty acid molecules—omega-3 fats in particular—in the precursor cells that prevented them from maturing into oligodendrocytes.
“Our study indicates that LPC omega-3 lipids act as factors within the brain to direct oligodendrocyte development, a process that is critical for brain myelination,” said David Silver, deputy director of the CVMD Program and the study’s senior author. “This opens up potential avenues to develop therapies and dietary supplements based on LPC omega-3 lipids that might help retain myelin in the aging brain—and possibly to treat patients with neurological disorders stemming from reduced myelination.”
Silver’s work has focused on lipid storage, transport, and metabolism with an eye toward translating findings into human treatments. In previous research, the Silver lab discovered Mfsd2a and collaborated with other investigators to understand the function of LPC lipid in the brain. The new research furthers this area of inquiry.
“We’re now aiming to conduct preclinical studies to determine if dietary LPC omega-3 can help to re-myelinate damaged axons in the brain,” added Silver. “Our hope is that supplements containing these fats can help to maintain—or even improve—brain myelination and cognitive function during aging.”













