A team of researchers from King’s College London and The Institute of Cancer Research have identified immune cell types that could be targeted for treatment of post-neoadjuvant chemotherapy (NAC)–resistant triple-negative breast cancer (TNBC) and ER+ HER2– breast cancer.
The research, published in Clinical Cancer Research, represented a “deep dive” into discovering the immunologic biomarkers within tumor tissues and blood samples of 153 early breast cancer patients (TNBC n=80; ER+HER2– n+73) who had residual cancer burden (RCB) after chemotherapy.
“Chemotherapy resistance in aggressive early breast cancers is a major reason why cancer regrows after treatment, contributing significantly to people not surviving their disease,” said lead author Sheeba Irshad, PhD, of Kings College London. “In order to find the right targets for drug developments, it’s important to have a deep understanding of the complex mechanisms that allow some cancer cells to resist treatment, then hide from our immune system to only re-emerge later when they’re harder to eradicate.”
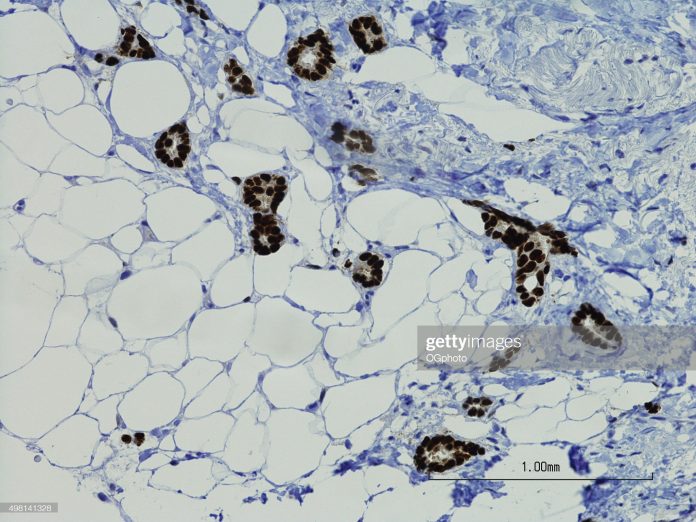
To investigate the immune environment that surrounds chemotherapy resistant tumors, the team investigated proteins and genes on both pre-treatment and post-treatment breast cancer tissue. They also measured how 1,330 cancer and immune-related genes within cancer tissues were affected by chemotherapy.
They found that chemotherapy resistant cancer cells had few immune cells around them, but chemotherapy did induce changes in several immune cell types. Specifically, they found increases in the number of “innate” (first responder) cells such as neutrophils and natural killer (NK) cells. NK cells help the body to fight infection and cancer. But analysis found the increased NK cells in patients with chemotherapy resistant disease lacked cytotoxic activity.
Irshad said that there were other findings of her team’s efforts that will require further investigation. The team observed downregulation of several stimulatory and inhibitory immune-checkpoint receptor expression (including PD-L1 and PD-1) which highlights the complexity of intervention with immunotherapies in the post-NAC adjuvant setting.
Researchers also found immune-related genes associated with NK cells were those associated with cell inhibition or exhaustion, which meant NK cells were unable to fight cancer cells. This new insight into the behavior of NK cells could be used to develop specific immunotherapies for these high-risk patients. This would need to be investigated in future clinical trials.
One important finding of their work was to show the potential to use liquid biopsies as an early monitoring method to determine whether patients are responding or not to their chemotherapy treatment regimen.
“We show chemotherapy-induced changes in the tumor microenvironment of TNBC residual disease, namely the depletion of B cells and enrichment of NK cells, are also reflected in the peripheral blood,” Irshad noted. “Our work has further identified features of peripheral immunity at baseline that are related to clinical outcomes after NAC treatment. Importantly, at baseline, patients with TNBC destined for a poor response to chemotherapy were found to have lower levels of the cytotoxic CD16+ NK cell population, which continued to remain depleted during chemotherapy.
This demonstrated that “monitoring of tumor immune dynamics longitudinally during chemotherapy is feasible and mirrors events within the tumor, and therefore may help to predict therapeutic response early, and potentially allow for tailoring of treatment prior to definitive surgery,” the researchers reported.
Finally, the investigation revealed several cell types that would be worth investigating further to understand how they are interacting with the resistant cancer cell and how they could be targeted as therapeutic interventions.













