A sequential drug treatment approach that can reverse the resistance of leukemia cells to tyrosine kinase inhibitor (TKI) treatment has been developed by scientists at Barts Cancer Institute at Queen Mary University of London.
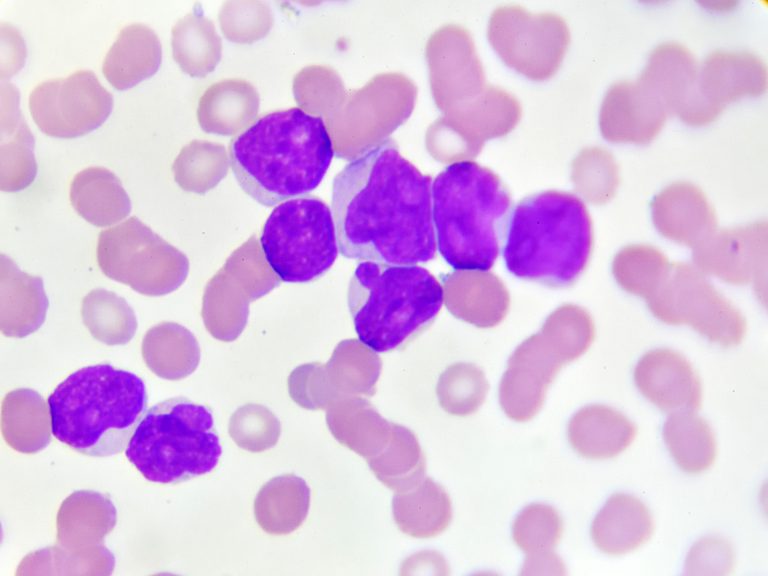
By rewiring the inner workings of the cancer cells and inhibiting a certain enzyme, the team was able to prime acute myeloid leukemia (AML) cells for sensitivity to treatment in the laboratory.
The team first characterized several epigenetic markers and enzyme networks that correlated with treatment resistance. They then found that inhibiting LSD1—an enzyme that creates one of these epigenetic markers—boosted activity of the MEK/MAPK pathway and left AML cells and patient samples vulnerable to subsequent treatment with the TKI trametinib.
Study lead Pedro Cutillas, PhD, from BCI’s Centre for Cancer Genomics & Computational Biology, explained, “Here, we found that intrinsic resistance to kinase inhibitors could be overcome by coercing kinase networks into pathways that are tolerant to drug sensitivity. By targeting LSD1 with a drug, we rewired the kinase network and left cancer cells unable to escape from treatment with the second drug, trametinib.”
“Overall, our study reveals the MEK pathway as a mechanism of resistance to LSD1 inhibitors in AML and shows a way to modulate kinase network circuitry to potentially overcome therapeutic resistance to kinase inhibitors.”
Kinase inhibitors are a type of targeted drug that block kinase enzymes—a kind of chemical messenger—within cells. Kinases activate proteins in cells that are needed for a variety of normal cellular functions, including metabolism, growth, division and survival; however, kinases can become dysregulated in cancer, helping cancer cells to grow and survive.
Although kinase inhibitors have shown success in the treatment of some tumor types, many cancers fail to respond or develop resistance against these targeted drugs. The authors stated, “Whereas some kinase inhibitors can substantially extend patient survival in some settings [such as drugs targeting the breakpoint cluster region protein–tyrosine kinase ABL1 fusion protein (BCR-ABL) in chronic myeloid leukemia], most of these agents produce transient responses and are only effective in a small number of patients.”
This relatively low overall clinical efficacy has been ascribed to tumor heterogeneity and to the existence of pathways that are able to compensate for target inhibition the team further noted. Kinase inhibitors work by blocking components of different signaling pathways that cancer cells use to grow and survive. However, similar to how satellite navigation devices suggest an alternative route to reach a destination if there is a road closure; cells can learn to use other routes to carry out a function when a drug blocks their usual pathway. These alternative routes, or ‘intrinsic resistance,’ compensate for the effects of the drug and can prevent the drug from killing the cancer cell.
However, the team stated, “Although the biochemical pathways and circuitries that cause resistance to targeted drugs are starting to emerge, the underlying genetic and epigenetic causes that mediate the activation and formation of such compensatory pathways and network topologies are less well understood.”
Building on previous work that investigated the mechanisms of resistance to drugs that target kinases, the team first treated leukemia cell lines with an experimental drug (GSK2879552) to block an enzyme called LSD1. LSD1 has a role in regulating gene expression in cells.
Their tests showed that blocking LSD1 inhibited the activity of one signaling pathway (called the PI3K/AKT pathway), but activated an alternative signaling pathway (named the MEK/MAPK pathway) that the leukemia cells were forced to utilize to survive.
As the leukemia cells were now relying on the MEK/MAPK pathway for survival, the team used a second drug—a kinase inhibitor called trametinib—to block that pathway. This effectively cut off all escape routes for the cells, which died.
The team used the same sequential treatment approach to treat blood cells collected from patients with acute myeloid leukemia, and found that the drug combination was effective at killing about 50 % of the AML samples. “Sequential LSD1i èMEKi treatments were particularly effective in about 50% of primary AML cases tested, suggesting that selection of patients for therapy may be required for successful therapeutic implementation,” the report noted.
Further experiments revealed that certain genetic changes and characteristics within the cancer cells influenced whether the cells were sensitive or resistant to the sequential treatment. “Primary human cells with KRAS mutations and those with high MEK pathway activity were the best responders to sequential treatment with LSD1 inhibitors then trametinib, whereas those with NRAS mutations and high mTOR activity were poor responders,” the investigators stated. Such characteristics may represent biomarkers that could help to predict the subpopulation of patients more likely to respond to this kind of treatment.
Drug resistance is a major barrier in the treatment of cancer and is responsible for the majority of cancer deaths. Trametinib has showed limited efficacy against leukemia in early phase clinical trials; however, this early-stage research has identified a way in which drug resistance to such kinase inhibitors may be reversed and potentially avoided. “Our results provide a rationale for using LSD1 antagonists to rewire the kinase networks of AML cells into topologies that are permissive to treatments with kinase-targeted drugs,” the authors concluded.
Cutillas added, “Instead of treating cancers with two or more drugs at the same time, as has been the main approach in previous research on drug combinations, our work suggests that sequential treatment with one inhibitor to create a new pathway dependency, followed by treatment with an inhibitor against the newly activated pathway may be an effective treatment strategy in leukemia.”
Cutillas and colleagues hope that this approach may be able to be translated into the clinic in the future, to increase the efficacy of drugs that by themselves have not shown significant clinical benefit. The team is also keen to explore whether the findings can be applied to other cancer types in addition to leukemia.
They pointed out, “The sequential treatment strategy differs from classical synthetic lethality approaches because, instead of cotreatments with two or more drugs, it aims to create new pathway dependencies by pretreating tumors with agents that change their biochemical circuitry, thus producing phenotypes susceptible to subsequent treatments with targeted drugs.” This approach has an immediate advantage in that it minimizes the potential for acquired resistance to emerge in sequentially treated cells,” the scientists noted.
Further work will be required to investigate the longer term effects of the treatment approach on both AML cells and normal cells and cell functioning, the team acknowledged. Nevertheless, they pointed out, “ … the results presented in this study highlight the sequential treatment with LSD1 inhibitors, followed by MEK kinase inhibitors as a new and potentially valuable strategy for the treatment of AML.”
Cutillas and colleagues reported on their findings in Science Signaling.













