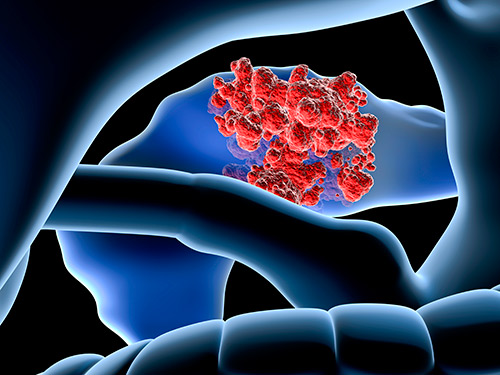
Research led by the Medical University Vienna shows that an image-based single-cell test could help improve therapy selection for patients with advanced blood cancers.
The approach involves testing cancer cells taken from the patient to assess the effects of a panel of different cancer drugs before the clinician makes a firm decision on which treatment pathway to follow for each patient.
“We wanted to enable true personalized medicine in cancer treatment,” explained study investigator Giulio Superti-Furga, a professor at the Medical University of Vienna, in a press statement.
“For years, many… have been working on ever-improving molecular profiles of genes, proteins and metabolites that should facilitate individualized treatment of patients. But the approach used here is a kind of a shortcut. We’re directly testing which drug actually works on the cancer cells.”
While personalized medicine has come a long way in the last decade, it still only provides new treatment opportunities for less than 10% of cancer patients. This new approach aims to add to the number of patients who can benefit by employing an ultra-tailored approach.
As reported in the journal Cancer Research, the investigators used an image-based single-cell functional precision medicine (scFPM) approach to guide cancer treatment in a group of 143 patients with advanced aggressive hematologic cancers including acute myeloid leukemia, aggressive B-cell non-Hodgkin lymphoma, and T-cell non-Hodgkin lymphoma. Each sample was tested with over 130 candidate drugs and the resulting effects observed.
Overall, 56 patients were given treatment that was suggested by the results of scFPM analysis. After two years of follow-up, over half the patients (54%) had a 30% improvement of progression-free survival compared with after their previous therapies. Twelve individuals had particularly good progression-free responses lasting three-times longer than would normally be expected.
“The idea of personalized cancer medicine is far from new. But many years of research have gone into developing the technology behind analyzing tumor tissue in such a way that therapy-relevant information can be extracted,” said Superti-Furga.
“Today, we can perform single-cell analyses of patient samples with unprecedented resolution and precision, observe individual immune cell interactions, and thus test the effect of an enormous variety of drugs.”
This kind of approach to precision cancer therapy has not been widely tested to date, but new technology such as the single cell analyses used in this study are making this kind of directed treatment possible.
“Our study demonstrates that individual therapy tailoring is feasible and effective in breaking resistance to prior therapies,” says Philipp Staber, lead author of the study and an associate professor at the Medical University Vienna.
“These platforms appear especially suited for hematological malignancies as primary patient material is more readily accessible as intact viable cells,” add the authors in the paper describing the research.













