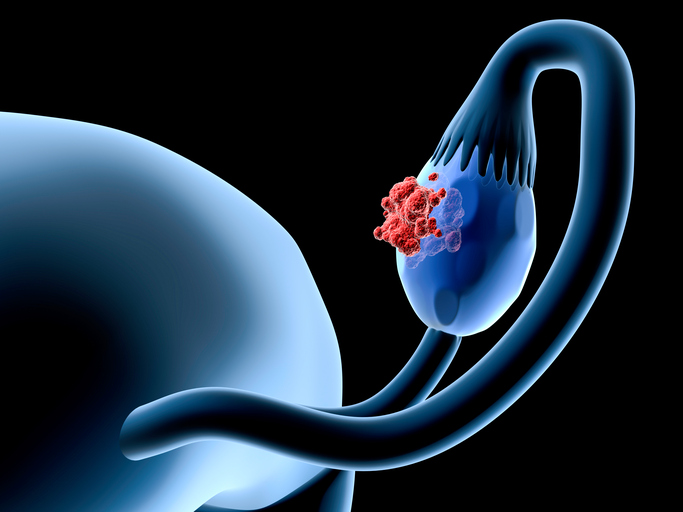
Ovarian cancer is the most lethal gynecologic malignancy and, despite their promise, immunotherapies have only modest efficacy against it. Now researchers at the University of Helsinki have uncovered new evidence about how tumor cells interact with the immune system in this particularly aggressive type of cancer, which affects about 240,000 women each year, leading to more than 150,000 deaths.
Using multiplex immunofluorescence and image analysis, the researchers characterized more than 110,000 individual cells from clinical ovarian cancer samples. They then investigated how the genetic characteristics of ovarian cancer affect how tumor and immune cells communicate with each other.
The study was published in Nature Communications this week.
The most common subtype of this disease is high-grade serous ovarian, peritoneal, or fallopian-tube cancer (HGSC), which causes 70-80% of all ovarian cancer deaths . The majority of HGSCs are deficient in homologous recombination (HR) DNA repair, most commonly due to mutations or hypermethylation of the BRCA1/2 genes.
These researchers set out to uncover how BRCA1/2 mutations shape the cellular phenotypes and spatial interactions of the tumor microenvironment. Using a highly multiplex immunofluorescence and image analysis, they generated spatial proteomic data for 21 markers in 124,623 single cells from 112 tumor cores originating from 31 tumors with BRCA1/2 mutation (BRCA1/2mut), and from 13 tumors without alterations in HR genes. They found a phenotypically distinct tumor microenvironment in the BRCA1/2mut tumors with evidence of increased immunosurveillance.
“With the help of this revolutionary imaging technology and advanced data analysis, we were able to study individual tumor cells, their functional properties and interactions with unprecedented precision,” says associate professor Anniina Färkkilä, the study’s corresponding author.
The single-cell imaging technology was developed in 2017 at Harvard Medical School, Färkkilä tells Inside Precision Oncology. Her lab has been using the technique since 2018.
“By studying individual cells directly in the tissue, we demonstrated how cancer cells hide in different ways, depending on the specific gene mutation. We found that the body’s immune system is more effective against tumors with a mutation in BRCA1/2 genes. By contrast, tumors without such mutations have a connective tissue barrier prohibiting the interaction between the cancer and immune cells,” says doctoral researcher Inga-Maria Launonen.
BRCA1/2 mutations occur in approximately 20% of poorly differentiated serous carcinomas. The researchers found that the killer T-cells closely guarded the aggressive tumor cells particularly in tumors with BRCA1/2 mutations, which could explain why these patients had a markedly better prognosis.
Notably, preliminary evidence suggests that HR-deficient tumors have a distinct tumor-immune microenvironment. BRCA1/2mut tumors have been predicted to contain more neoantigens than tumors with no alterations in genes of the HR pathway (HRwt), harbor an increased number of tumor-infiltrating lymphocytes, and have an elevated PD-L1 expression as compared to HR- proficient tumors
The researchers reported a prognostic role of a proliferative tumor-cell subpopulation, which was linked to enhanced spatial tumor-immune interactions by CD8+ and CD4 + T-cells in the BRCA1/2mut tumors. The single-cell spatial landscapes indicate distinct patterns of spatial immunosurveillance, with the potential to improve immunotherapeutic strategies and patient stratification in HGSC.
“By increasing our understanding of how tumor genes trick the immune system, we will be able to develop more effective ways to activate the body’s own immune defenses to kill the cancer cells,” Launonen says.
The results of the study, the researchers say, confirm the significance of the interaction between tumor and immune cells in identifying new and more effective therapies as well as in choosing the right therapy for each patient.
“Our findings will enable us to tailor precision immuno- and combination therapies that have the potential to even cure ovarian cancer in the future,” Färkkilä says.













