Researchers at Case Western Reserve University showed that a stem cell-based therapy has promise for treating resistant and chronic lung infections with non-tuberculosis mycobacteria.
Using a human cell line and a mouse model, the research team demonstrated that human marrow‐derived mesenchymal stem cells (MSCs) have antimicrobial and anti-inflammatory activity against Mycobacterium avium and/or M. intracellulare.
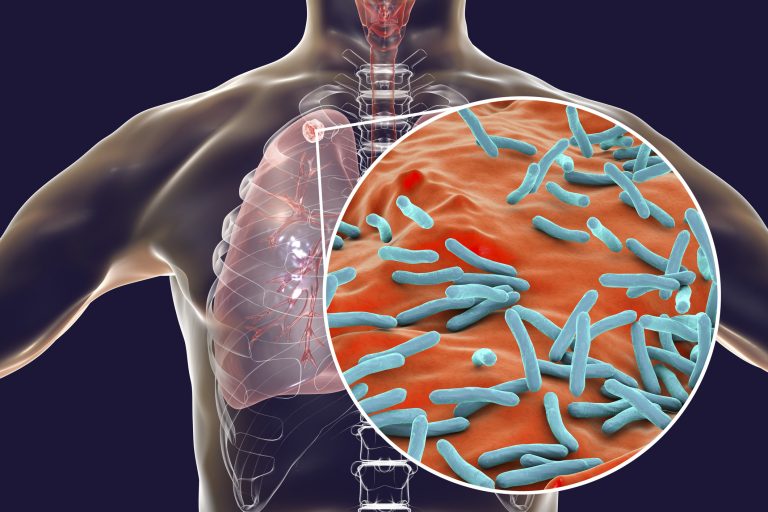
Mycobacteria is a common genus of bacteria mostly known for causing tuberculosis—M. tuberculosis—and also leprosy—M. leprae. However, there are several other species in this group that can also cause chronic lung disease, including M. avium and M. intracellulare, in some people, often in vulnerable individuals such as those with cystic fibrosis. In the U.S. alone there are over 100,000 people living with this type of infection.
“Non-tuberculosis mycobacteria infections can be very difficult to resolve,” said Tracey Bonfield, Ph.D., an associate professor at Case Western and the first author of the article describing the work, which is published in the journal STEM CELLS Translational Medicine.
“Treatment typically requires taking multiple antibiotics, often for years. Patients who suffer from chronic NTM infection not only deal with the consequences of the disease, but also the toxicity, as well as inefficiency and side effects of the antibiotics used to treat it.”
Using a human cell line and a mouse model of this type of infection, Bonfield and co-authors showed that marrow-derived MSCs have potential to treat this kind of chronic infection. They have direct antimicrobial activity, secreting antimicrobial ‘helper’ molecules such as CCL20 and IL-6, among others, that help the body to fight off the infection.
They can also increase the efficacy of antibiotic treatment, meaning that less of the drugs might be needed to treat such a chronic infection. This could in turn help reduce toxic side effects associated with this treatment.
The team cautions that there is likely to be variability in efficacy of stem cell antimicrobial and anti-inflammatory effects depending on the donor of the cells. Levels of helper immune molecules such as CCL20 and IL-6 varied between donors and seemed to have a direct impact on the antimicrobial activity of the cells.
“Every donor human MSC preparation has a unique profile in terms of response to pathogens, which likely translates into the downstream events related to successful potency and host response to treatment,” write the authors.
“Future studies are planned to evaluate unique human MSC fingerprints associated with antimicrobial potency and whether it is global or pathogen specific,” they conclude.
The team behind this study have previously shown that human MSCs have the potential to treat other types of lung infections such as those caused by Pseudomonas aeruginosa and Staphylococcus aureus, but this is the first study applying this knowledge to target mycobacterial infections.











