Promising biomarkers for progression of non-alcoholic fatty liver disease (NAFLD) were found in a study led by researchers at the Translational Genomics Research Institute (TGen), an affiliate of City of Hope.
They identified differences in DNA methylation (DNAm) that accurately predicted different stages of liver fibrosis in as many as 94% of patients with NAFLD, according to the study published in the journal Clinical Epigenetics.
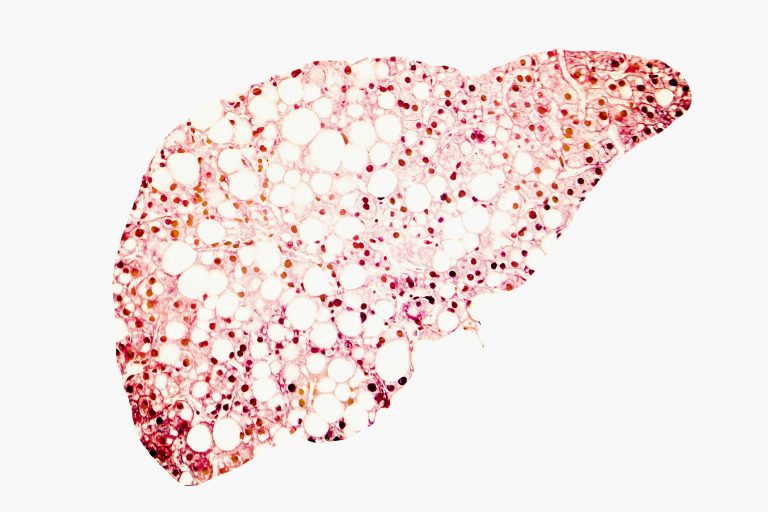
NAFLD is the most common chronic liver disease among Western nations, characterized by accumulations of fat in the liver. This condition can include development of fibrosis, which may be caused by DNA methylation (DNAm)—a biological process in which methyl groups are added to DNA without changing its sequence.
“DNAm patterns can be used to identify distinct cell types in the liver, and changes in cell-type composition,” said Johanna DiStefano, PhD, head of TGen’s Diabetes and Fibrotic Disease Unit. She is also one of the study’s senior authors.
Using samples retrieved by biopsies, researchers examined genomic data from 325 NAFLD patients: 206 with no apparent liver scarring and 119 with varying levels of fibrosis. In its most severe form, NAFLD can progress to a condition called nonalcoholic steatohepatitis (NASH), and in turn lead to cirrhosis, cancer of the liver, and death.
The researchers found that more severe fibrosis levels were associated with a progressive increase in the percentage of immune cells in the liver, and a corresponding decrease in the percentage of epithelial cells, a type of cell that lines various body surfaces, including organs such as the liver.
Karen Conneely, PhD, Associate Professor in the Department of Human Genetics at the Emory University School of Medicine, and a senior author of the study, explained that researchers also found that even after accounting for differences in cellular composition between individuals, DNAm levels at specific sites in the genome were decreased in patients with severe fibrosis.
The differences were striking enough that Emory’s Nicholas Johnson, PhD, and a lead author of the study, was able to develop a model based on DNAm at 28 genomic sites that could accurately predict fibrosis levels in 94% of NAFLD patients in an independent test set.
“These findings are consistent with DNAm as a mechanism underpinning, or marking, fibrosis-related shifts in cell composition, and demonstrate the potential of DNAm as a possible biomarker of NAFLD fibrosis,” said Xiumei Wu, PhD, a TGen Staff Scientist in the DiStefano Lab, and one of the study’s authors.
For this study, samples were drawn directly from patient livers via the relatively invasive use of biopsies. Taking advantage of technology pioneered by TGen, they suggest that future samples might be obtained from circulating blood.
“Circulating DNAm has been suggested as a potential noninvasive biomarker of disease severity for NAFLD,” the researchers wrote. “These results suggest that our model could potentially predict NAFLD fibrosis in blood DNAm.”
The researchers suggest that future analysis also could be complemented by using single-cell RNA sequencing, a more exacting method of analyzing genomic information, which has the potential to measure cell composition at a higher resolution, and facilitating a greater understanding of the relationship between NAFLD fibrosis, cellular composition, and DNAm.
“Overall, our investigation shows that DNAm provides information that is not only useful for understanding the underlying biology of NAFLD,” DiStefano said, “but may also serve as a clinical tool capable of independently diagnosing fibrosis.”













