New research published in Nature Cancer from investigators at the University of Texas MD Anderson Cancer Center shows that a combination of immunotherapies targeting both T cells and myeloid suppressor cells was able to reprogram the tumor immune microenvironment and improved anti-tumor response in pancreatic cancer models.
The team used comprehensive immune profiling in mouse and human pancreatic cancers to systematically identify mechanisms of immunotherapy resistance and investigate potential therapeutic targets. They found that neutralizing several distinct immunosuppressive mechanisms of the TIME dramatically improved survival rates in laboratory models, pointing to a potential treatment option for pancreatic cancer, which is a deadly, and notoriously unresponsive cancer.
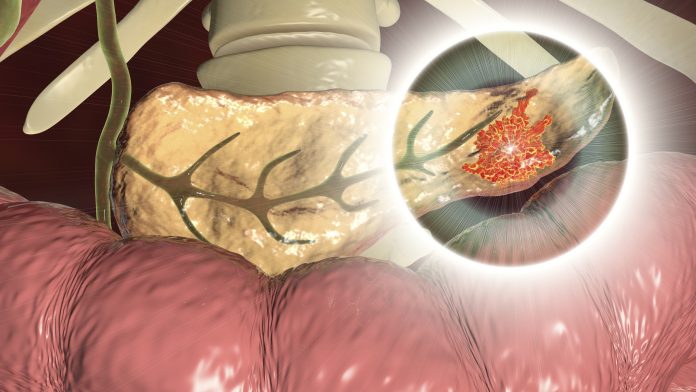
Pancreatic cancer is one of the leading causes of cancer death in the United States, in part because 80% of cases are diagnosed at an advanced stage. Pancreatic cancer is also considered to be “non-immunogenic,” meaning it is unresponsive to commonly used anti-PD-1 and anti-CTLA-4 immune checkpoint inhibitor therapy (ICT). While this is partly due to the immunosuppressive conditions in the TIME, the mechanisms behind this resistance are not fully understood. However, the researchers wrote, ”Several preclinical and early-phase clinical trials have shown ‘signals of activity’ with immunotherapy combinations, encouraging further investigation. It is tempting to speculate that rational combinatorial treatments targeting nonredundant mechanisms of immune resistance may enhance the efficacy of ICT in PDAC.”
By testing antibodies targeting these checkpoints, the researchers found that models treated with a 41BB agonist and LAG3 antagonist in combination exhibited slower tumor progression, higher levels of antitumor immunity indicators, and significantly improved survival rates, compared with animals treated using each antibody either alone or alongside other checkpoint inhibitors. Notably, these preclinical studies faithfully mirrored the human data in their lack of efficacy of anti-PD1 or anti-CTLA-4 therapy.
Because the dual-therapy combination did not completely eliminate established tumors, the investigators also examined efforts to reprogram the TIME to further sensitize tumors to immunotherapy. At baseline, the TIME contained an abundance of myeloid-derived suppressor cells (MDSCs) expressing CXCR2, a protein associated with recruiting immunosuppressive cells. Inhibiting CXCR2 alone decreased MDSC migration and blocked tumor growth, but it was not curative. This prompted the investigators to consider a combination targeting 41BB, LAG3, and CXCR2.
It was this triple combination that resulted in complete tumor regression and improved overall survival in 90% of preclinical models. In a more stringent lab model that develops multiple spontaneously arising tumors with higher treatment resistance, the combination achieved complete tumor regression in over 20% of cases. “In contrast with anti-PD-1 and anti-CTLA4, agonist 41BB and antagonist LAG3 treatment reprogrammed the TIME toward antitumor immunity with increased T cell subsets with antitumor effects, increased T cell clonality and diversification, decreased immunosuppressive myeloid cells and increased antigen presentation and decreased the immunosuppressive capability of remaining myeloid cells,” the authors commented. “The addition of therapy targeting CXCR1/2 on neutrophilic/granulocytic MDSCs revealed that effective immune treatment is possible in PDAC but requires neutralization of distinct immunosuppressive mechanisms.”
The researchers also confirmed that the two therapeutic targets are present in human pancreatic cancer samples. “… we found that 81% of patients with PDAC have 41BB-expressing T cells, while 93% of patients with PDAC have LAG3-expressing T cells, suggesting that these targets may be relevant for a meaningful fraction of patients with PDAC,” they wrote. “In this context, it is noteworthy that the majority of ongoing immunotherapy trials in PDAC employ PD-1 and/or CTLA4 as the ICT backbone, including trials combining ICT with CXCR2 antagonists.”
DePinho added. “These are encouraging results, especially considering the lack of effective immunotherapy options in pancreatic cancer. By targeting multiple synergistic mechanisms that get in the way of the immune response, we can give T cells a fighting chance to attack these tumors. Of course, we still need to see how this combination translates into a safe and effective regimen in the clinic, and we invite other researchers to build upon these results. We are optimistic that pancreatic cancers, and hopefully other non-immunogenic cancers, can ultimately be rendered vulnerable to combination immunotherapy.”
The authors point out that these particular immunotherapy agents currently are undergoing clinical trials as monotherapies, suggesting potential opportunities to rapidly translate this triple combination into clinical studies. Nevertheless, they acknowledged, “As with all preclinical model systems and human biospecimen correlations, prospective clinical trials will be needed to substantiate the hypothesis generated from this work.”













